Digital subtraction angiography (DSA)

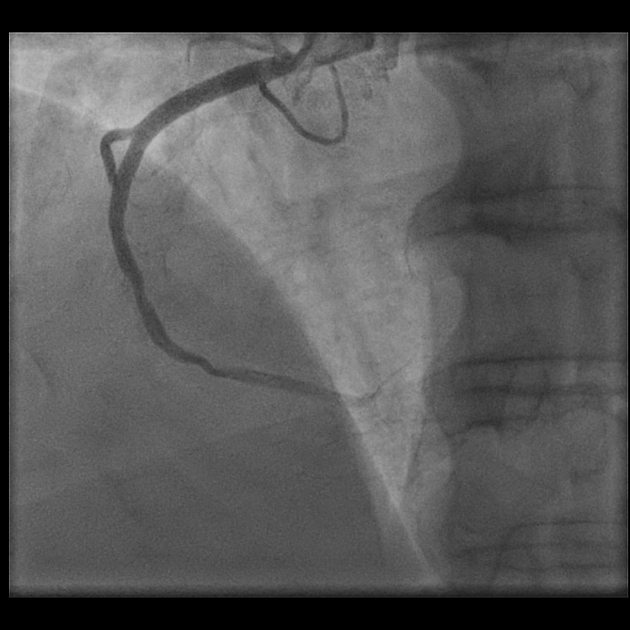

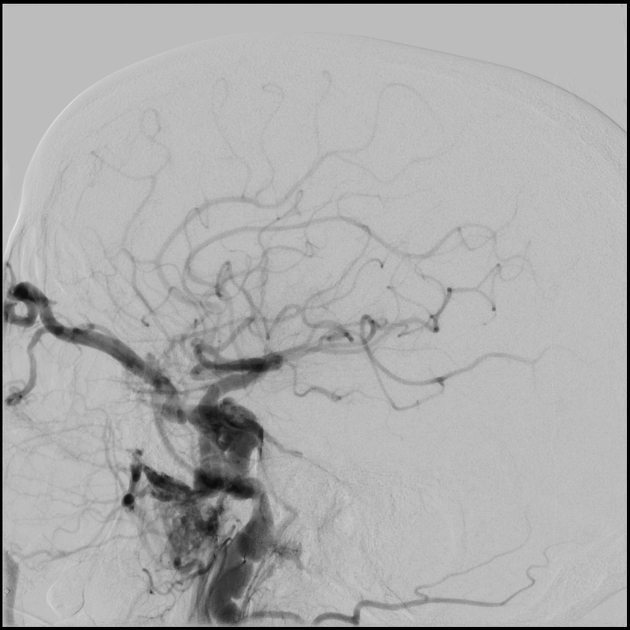
Digital subtraction angiography (DSA) is a fluoroscopic technique used extensively in interventional radiology for visualizing blood vessels. Radiopaque structures such as bones are eliminated ("subtracted") digitally from the image, thus allowing for an accurate depiction of the blood vessels.
History
Angiography is largely possible thanks to the Seldinger technique (first described in 1953) for intravascular access.
Digital subtraction angiography, whereby a pre-contrast image is acquired, then subtracted from subsequent post-contrast images, was made possible in the 1970s, thanks to real-time refreshing of the resulting images.
Indications
There are numerous indications for angiography and their number has been on the rise ever since interventional radiology has been shown to successfully supplant many open vascular procedures. Salient examples include:
- endovascular aneurysm repair
- arterial balloon angioplasty
- arterial stenting
- endovascular embolization
- thrombectomy
Contraindications
Renal insufficiency and hypersensitivity to iodinated contrast media are relative contraindications. Some centers use carbon dioxide as a contrast agent for these cases.
Procedure
Preprocedural evaluation
Patient evaluation should include, but is not limited to:
- presence of atherosclerotic disease (e.g. prior myocardial infarction)
- diabetes
- renal function status
- medications
- allergies and previous exposure to iodinated contrast media
- prior surgical procedures, especially vascular
- reports from previously performed angiograms, if any
- review of any relevant vascular imaging studies, e.g. preprocedural CT angiogram
See also: patient safety checklist.
Positioning/room set up
The angiography suite must be equipped with a crash cart and monitoring equipment. Patient heart rate and blood oxygenation are monitored continuously, while blood pressure is measured intermittently via a self-inflating cuff.
All procedures should be performed under strict aseptic conditions, including attire, technique and preparation.
Depending on the procedure and the patient's condition, an anesthesiologist may be required to administer conscious sedation or even general anesthesia.
The patient can be positioned with their head on either end of the bed to facilitate convenience of vascular access and maneuvering for the interventional radiologist.
Equipment
The fluoroscopy unit consists of a C-arm unit that can be rotated axially and sagittally around the floating-top table. The distance between the X-ray tube and the image intensifier can be adjusted, as can collimation and several other parameters. In dedicated angiography units, there is a second set of controls for the angiographer (radiographer).
A modern angiography unit has all of the following features :
- collimators (including oblique) and filters for dose reduction
- pulsed fluoroscopy with a variety of frame rates for dose reduction
- ability to change and display collimator position without fluoroscopy
- road mapping and landmarking
- last image hold and frame-grab
- display of images side-by-side
- masks
- image enhancement
- different image manipulations
- cine
- measurements and quantification (e.g. of the degree of arterial stenosis)
The image is at least a 1024 x 1024 pixel matrix. Most modern medical displays are flat screens; some of the detectors are flat panel.
Technique
DSA technique
Digital subtraction angiography is used to produce images of the blood vessels without interfering shadows from overlapping tissues. This provides a clear view of the vessels and allows for a lower dose of contrast medium .
- the non-contrast image (mask image) of the region is taken before injecting contrast material and therefore shows only anatomy, as well as any radiopaque foreign bodies (surgical clips, stents, etc.) as would a regular x-ray image.
- contrast images are taken in succession while contrast material is being injected. These images show the opacified vessels superimposed on the anatomy and are stored on the computer.
- the mask image is then subtracted from the contrast images pixel by pixel. The resulting subtraction images show the filled vessels only.
- recording can continue to provide a sequence of subtracted images based on the initial mask.
- the subtraction images can be viewed in real-time. Even if the patient lies still, there is bound to be some degree of misregistration of images due to movement between the acquisition of the mask image and the subsequent contrast images. The effect is prominent at high-contrast interfaces, such as bone-soft tissue, metal staples and coils, and bowel air. Pixel shifting (either manual or automatic), i.e. moving the mask retrospectively, can minimize misregistration, but focal movement such as bowel peristalsis, will not be corrected.
It should be noted that since image subtraction causes a decrease in signal-to-noise ratio, the subtraction images appear noisier than the source images. The inevitable solution to this is to increase mA. There are also algorithms in place for reducing scatter.
Procedural technique
For every purpose, there is at least one technique, but common to them all is the application of DSA for visualization:
- the patient lies on the angiography table
- local anesthesia is administered at the intended puncture site (usually lidocaine hydrochloride 1% or 2% w/v)
- in certain procedures (e.g. a child undergoing cerebral angiography), general anesthesia is performed
- the Seldinger technique is used to gain access to a blood vessel
- ultrasound is often used for visualizing the vessel in real-time for puncturing
- a standard access kit includes a straight 18 gauge needle and .035" guidewires, on which the diagnostic and therapeutic catheters are threaded
- in many cases, a micro-introducer access kit (.018" guidewire threaded through a 21 gauge initial access needle) is used for access, either for the entire procedure or to be replaced with the standard kit. Using a micro-introducer facilitates less traumatic entry and can be retrieved without massive bleeding should there be a need for re-puncturing
- on procedure completion, hemostasis is applied to the puncture site
Postprocedural care
This depends on the nature of the procedure and whether it was performed on an inpatient or outpatient basis.
Patient should be immobilized for 4-6 hours and keep on supine position. Frequent observations should be done to look for puncture site hematomas, which is the commonest complication.
Complications
Complications can be categorized into local and systemic complications:
Local complications (puncture site):
- from the puncture site (commonest complication)
- thrombus formation
- local tissue damage
- pseudoaneurysm
- arteriovenous fistula
Systemic complications:
- thromboembolism
- air embolism
- vessel dissection
- contrast mediated nephrotoxicity
See specific procedures for specific complications.

