hepatic abscess
























































Hepatic abscesses, like abscesses elsewhere, are localized collections of necrotic inflammatory tissue caused by bacterial, parasitic, or fungal agents.
Epidemiology
The frequency of individual infective agents as causes of liver abscesses are intimately linked to the demographics of the affected population:
- in developing countries, parasitic abscesses are the most common
- in developed countries, liver abscesses are rare in healthy individuals, with imported infections from visits overseas accounting for the majority of cases
Risk factors
In developed countries, bacterial abscesses are most common, usually in the setting of comorbidities such as:
- infection elsewhere (most common)
- abdominal sepsis most common
- necrotizing enterocolitis (portal venous drainage)
- immunocompromised
- diabetes mellitus found in up to 15% of patients with hepatic abscess
- HIV/AIDS
- elderly
- chemotherapy/transplant recipients
- malignancy
- end-stage renal disease
- intravenous drug use
- trauma
- ERCP
- cryptogenic: 15%
- liver cirrhosis
- hepatic artery bacteremia
- biliary disease
- inflammatory bowel disease
- pancreatic disease
- perforated duodenal ulcer
Clinical presentation
The typical presentation is one of right upper quadrant pain, fever, and jaundice. Anorexia, malaise and weight loss are also frequently seen. Depending on the immune status of the patient, and the organism involved, the presentation may be dramatic or insidious.
Pathology
Hepatic abscesses can occur via different routes such as :
- haematogenous spread of infection via the portal vein or hepatic arteries
- biliary spread of infection from ascending cholangitis or cholecystitis
- direct inoculation in the setting of penetrating trauma or iatrogenic following a procedure
Bacteria
Most abscesses in this setting are polymicrobial, with the most common bacterial agents being :
- gram-negative aerobic and anaerobic organisms
- Escherichia coli
- Klebsiella pneumoniae
- the hypervirulent Asian strain has a particular predilection
- Bacteroides
- gram-positive
- anaerobic and microaerophilic streptococci
- enterococci
Parasites
Parasitic abscess in patients from developing countries include:
- amoebae: amoebic hepatic abscess (anchovy paste appearance of drained contents)
- echinococcal (hydatid disease of the liver): this will be discussed separately
- protozoa
- helminths
Radiographic features
As a general rule, bacterial and fungal abscesses are often multiple, whereas amoebic abscesses are more frequently single. Amoebic abscesses are more common in a sub-diaphragmatic location and are more likely to spread through the diaphragm and into the chest.
When the infection spreads to the liver through the portal veins it arises more commonly in the right lobe, probably due to an unequal distribution of superior and inferior mesenteric vein contents within the portal venous distribution.
Plain radiograph
A plain abdominal radiograph is not sensitive for evaluating liver abscesses. Indirect signs visible include:
- gas within the abscess or biliary tree (pneumobilia) or beneath the diaphragm
- right-sided pleural effusion
Ultrasound
Liver abscesses are typically poorly demarcated with a variable appearance, ranging from predominantly hypoechoic (with some internal echoes) to hyperechoic. Gas bubbles may also be seen . Color Doppler will demonstrate the absence of central perfusion.
Contrast-enhanced ultrasound shows wall enhancement during arterial phase and progressive washout during portal or late phases. The liquefied necrotic area does not enhance. The use of contrast allows one to characterize the lesion, measure the size of the necrotic area, and depict internal septations for management purposes. In small abscesses (under 3 cm) and in highly septated abscesses, drainage is not recommended.
In patients with monomicrobial K. pneumoniae abscesses, the lesion may appear solid and mimic a hepatic tumor .
CT
As with other modalities, the appearance of liver abscesses on CT is variable. In general, they appear as peripherally enhancing, centrally hypoattenuating lesions . Occasionally they appear solid or contain gas (which is seen in ~20% of cases ). The gas may be in the form of bubbles or air-fluid levels . Segmental, wedge-shaped or circumferential perfusion abnormalities, with early enhancement, may be seen .
The "double target sign" is a characteristic imaging feature of hepatic abscess demonstrated on contrast-enhanced CT scans, in which a central low attenuation lesion (fluid-filled) is surrounded by a high attenuation inner rim and a low attenuation outer ring . The inner ring (abscess membrane) demonstrates early contrast enhancement which persists on delayed images, in contrast to the outer rim (edema of the liver parenchyma) which only enhances the delayed phase .
The "cluster sign" is a feature of pyogenic hepatic abscesses . It is an aggregation of multiple low attenuation liver lesions in a localized area to form a solitary larger abscess cavity.
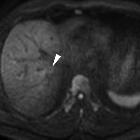
MRI
Signal characteristics include:
- T1
- usually hypointense centrally
- heterogeneous
- maybe slightly hyperintense in fungal abscess
- T2
- tends to have hyperintense signal
- perilesional edema manifests as high signal intensity on T2-weighted images and can be identified in 35% of liver abscesses
- T1 C+ (Gd)
- enhancement of the capsule, although this may be absent in immunocompromised patients
- multiple septations may be visible
- DWI: tends to have high signal within the abscess cavity , and high signal at the periphery
- ADC: tends to have low signal within the abscess cavity , and high signal at the periphery
Treatment and prognosis
Medical antimicrobial therapy is required in all cases and sometimes suffices if abscesses are small.
Radiology has a major role to play in the percutaneous drainage of hepatic abscesses, which can be performed either under ultrasound or CT guidance.
Surgery is limited to those patients where percutaneous drainage is impossible or has proven ineffective. Additionally, the source of the abscess may require surgical treatment at which time the abscess may also be drained.
Prognosis is highly variable, depending not only on the organism involved and size of the abscess but also on the comorbidities present. Figures range from 9-80% .
Complications
- hepatic vein thrombosis: ~22%
- portal vein thrombosis: ~24%
- rupture into:
- right subphrenic space
- abdominal cavity
- pericardium
- gastrointestinal tract
- sepsis
- thrombosis of the inferior vena cava
Differential diagnosis
General imaging differential considerations include:
- malignancy: usually greater diffusion restriction at the periphery (lower ADC values)
- mass-forming cholangiocarcinoma
- necrotic metastases: cystic lesions are usually not clustered or septated
- hepatocellular carcinoma: more heterogeneous, irregular infiltrating border in the setting of cirrhosis
- hemorrhagic liver cysts can appear multiloculated
- biliary cystadenoma
- hepatic peliosis
- hydatid cyst: large cystic liver mass with peripheral daughter cysts
- hepatic hemangioma
- hepatic adenoma
- hepatic infarct: peripheral, segmental distribution, wedge-shaped
Siehe auch:
- hepatozelluläres Karzinom
- Lebermetastasen
- akute Cholezystitis
- Differenzialdiagnosen zystischer Leberläsionen
- simple Leberzyste
- Peliosis hepatis
- Gas in der Leber
- nekrotische Lebermetastasen
- Abszess durch Escherichia coli
- Escherichia coli
und weiter:
- hypodense Leberläsionen
- Abszess
- Biliom
- cholangiozelluläres Karzinom
- Askariden
- fokale Leberverfettung
- zystische Lebermetastasen
- multifokale noduläre Steatosis hepatis
- biliäres Zystadenom
- differential diagnosis for a focal gas collection in the right upper quadrant
- Abszess Sonographie
- multiple amebic hepatic abscesses communicating with the biliary tree
- mesenchymales Leberhamartom
- infizierte Leberzysten
- post-traumatic hepatic abscess
- multiple hypodense Leberherde
- hepatic Fascioliasis
- multiple pyogenic hepatic abscesses
- liver abscess with spontaneous drainage in the peritoneal cavity complicating the ethanol injection therapy of HCC
- chologene Leberabszesse
- liver abscess drainage
- Amöbenabszess der Leber
- biliogener Abszess
- hepatogastrische Fistel
- abdomineller Abszess

 Assoziationen und Differentialdiagnosen zu Leberabszess:
Assoziationen und Differentialdiagnosen zu Leberabszess:






