vagus nerve






The vagus nerve is the tenth (X) cranial nerve and provides the bulk of the parasympathetic input to the gastrointestinal system and to the heart. It is a complex mixed sensory, motor and parasympathetic nerve.
Gross anatomy
Central connections
The vagus nerve arises as multiple rootlets at the posterolateral sulcus of the medulla, between the inferior cerebellar peduncle and inferior olivary nucleus.
There are four cranial nerve nuclei that contribute to the vagus nerves:
- two motor nuclei:
- nucleus ambiguus: branchial motor fibers
- dorsal vagal nucleus: parasympathetic motor fibers (visceral efferent)
- two sensory nuclei:
- solitary tract nucleus: visceral sensory (taste)
- spinal trigeminal nucleus: general sensory (cutaneous)
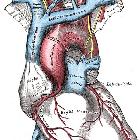
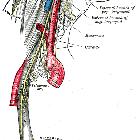
Course
Fibers from the central nuclei exit/enter the medulla at the postolivary sulcus, in between the glossopharyngeal nerve (CN IX) and the cranial root of accessory nerve (CN XI). From here, the vagus nerve travels through the basal cistern to exit the skull through the pars vascularis part of the jugular foramen to enter the carotid space. Within the jugular fossa lies the superior (jugular) sensory ganglion of the vagus nerve and the inferior (nodose) ganglion, which lies approximately 1 cm distally.
The vagus nerve descends vertically through the neck within the carotid sheath, where it lies posteriorly between the internal/common carotid artery and internal jugular vein.
Since the thorax is not symmetrical, the course of the left and right vagus nerves is not identical.
The left vagus nerve crosses anterior to the left subclavian artery as it enters the thorax. It passes lateral to the aortic arch as it descends posterior to the hilum of the left lung and towards the esophageal hiatus, which it passes through to enter the abdominal cavity.
The right vagus nerve also passes anterior to the right subclavian artery before diving into the fat surrounding the innominate vessels. It reaches the right paratracheal region before descending, like the left, posterior to the lung hilum and then medially to the esophageal hiatus, which it passes through to enter the abdominal cavity.
Near the esophageal hiatus the left and right vagus nerves meet and join to form the esophageal plexus, from which an anterior and posterior vagal trunk (also called gastric nerves) form and descend into the abdomen. The trunks are not composed of equal fibers from the left and right as the anterior trunk is mainly composed of fibers from the left.
Branches
The branches of the vagus nerve are described below, starting with the proximal branches and moving distally.
From the superior ganglion:
- small meningeal nerve
- auricular nerve (Arnold nerve)
- small communicating branches
From the inferior ganglion:
- pharyngeal nerve which supplies the pharyngeal plexus
- supplies the superior, middle and inferior pharyngeal constrictor muscles, palatopharyngeus, salpingopharyngeus, levator veli palatini, palatoglossus and the muscle of the uvula
- carotid body branches
- superior laryngeal nerve which divides into the:
From the vagus nerve:
- recurrent laryngeal nerve
- superior and inferior cardiac nerves
- anterior and posterior bronchial nerves
- esophageal plexus
- gastric nerves
- celiac plexus: from the right vagus
- hepatic plexus: from the left vagus
Radiographic features
CT
First-line choice for imaging investigation for distal vagal neuropathy. Contrast-enhanced images from hyoid bone to mediastinum should be obtained.
Bony reformat CT of the skull base may be beneficial as an adjunct study to MRI for imaging proximal vagal neuropathy.
MRI
First-line choice for imaging investigation of proximal vagal neuropathy. Sequences should include T1W, T2W, contrast-enhanced T1W FS in axial and coronal planes and images acquired should extend from the medulla to hyoid bone.
Related pathology
The vagus nerve can be affected by pathology from its origin to anywhere along its course.
Clinical presentation
As the vagus nerve is mostly parasympathetic, sensory clinical features can be subtle or absent; especially when affected below the origin of the recurrent laryngeal nerves. Features include :
- deviation of the uvula away from the affected side
- ipsilateral loss of pharyngeal reflex
- ipsilateral vocal cord paralysis
Supranuclear lesions
Supranuclear lesions affecting the vagus often involve other cranial nerves as well, including cranial nerves IX, XI and XII. Unilateral lesions typically reveal little or no deficit due to the bilateral input to the nucleus ambiguus from the corticobulbar regions. Pseudobulbar palsy can occur when there are bilateral corticobulbar lesions.
Brainstem lesions
Brainstem lesions that may affect the vagus include:
- brainstem neoplasms
- demyelinating/inflammatory disease
- vascular disease
- syringobulbia
- Avellis syndrome
Jugular foramen lesions
- jugular foramen syndrome (Vernet syndrome)
- fractures involving the base of the skull
- neoplasms involving the base of the skull
- neoplasms within the jugular foramen such as glomus jugulare, meningioma and schwannoma
Extracranial lesions
- vagus nerve mononeuritis
- trauma
- infiltration by tumor
- primary tumors of the vagus nerve
- vagal schwannoma
- vagal neurofibroma
History and etymology
Vagus is Latin for wandering, named because of the long, wandering course of the nerve; the same Latin root gives rise to the English word, a vagrant.
Siehe auch:
und weiter:

 Assoziationen und Differentialdiagnosen zu Nervus vagus:
Assoziationen und Differentialdiagnosen zu Nervus vagus:


