intraductal papilloma of breast

















Intraductal papillomas are the most common masses within the milk ducts of the breast. They are benign tumors but may contain areas of atypia or carcinoma. The most common symptom is nipple discharge.
Epidemiology
- sex
- almost exclusively in women
- extremely rare in males
- age
- classically most common during 40-50 years of age (average 48 years old)
- increasing use of breast ultrasound has resulted in more frequent detection of papillary lesions in younger, asymptomatic women
Clinical presentation
- often asymptomatic (incidental imaging finding)
- nipple discharge: especially if unilateral, spontaneous, persistent
- bloody or clear (serosanguineous) nipple discharge, often less than six months duration
- more common in central versus peripheral papillomas
- bloody nipple discharge is thought to be due to twisting of the papilloma on its fibrovascular pedicle, leading to necrosis, ischemia, and intraductal bleeding
- bloody nipple discharge may have higher association with atypical or malignant lesions
Pathology
Papillomas are proliferative tumors originating from the walls of milk ducts, typically growing within the duct and tending to cause local ductal obstruction. They are composed of monotonous epithelial/myoepithelial cells encompassing a papillary fibrovascular core, and characteristically grow to form smooth well-circumscribed nodules.
Papillomas are typically small (<10 mm) lesions but may range from 3 mm to >2 cm . They most commonly occur ~3.5 cm from the nipple but may occur anywhere from anterior to posterior depth .
Increasingly, the central question in the assessment of breast papilloma is whether there is any evidence of cellular atypia. Any finding suggestive of more than merely benign proliferation are generally grounds for surgical excision of the entire lesion. In addition, papillomas have been reported occurring adjacent to other significant lesions such as atypical ductal hyperplasia or DCIS.
Papillomas may be solitary or multiple. Multiple papillomas, especially more than 5 lesions, are considered papillomatosis. There may be a higher rate of associated malignancy with multiple papillomas.
Subtypes
Location
They may be classified by location:
- central: within a major subareolar duct, often solitary
- peripheral: occur within the terminal duct lobular unit, may be multiple
Radiographic features
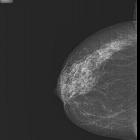
Mammography
Mammograms are frequently normal (particularly with small intraductal papillomas). When imaging findings are present, they include solitary or multiple dilated ducts, a circumscribed benign-appearing mass (often subareolar in location), or a cluster of calcifications.
Galactography
Galactography usually reveals a filling defect or other ductal abnormalities, such as ectasia (usually between the nipple and filling defect), obstruction, or irregularity. However, these findings are non-specific.
Galactography may outline the number, location, extent, and distance from the nipple.
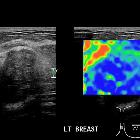
Breast ultrasound
Papilloma may be seen as a well-defined solid nodule or intraductal mass which may either fill a duct or be partially outlined by fluid - either within a duct or by forming a cyst. Color Doppler will demonstrate a vascular stalk.
A dilated duct can be frequently visible sonographically.
MRI
Most commonly appear as modestly-T2-bright, circumscribed, solid enhancing lesions. Morphological characteristics on MR may be quite variable:
- shape: can be oval/round (~75%) or irregular (~25%) shape
- margin: smooth or irregular (spiculation suggests malignancy)
- consistency: mostly solid (~90%), but can be cystic or complex cystic
Signal characteristics
- T1: isointense to slightly hypointense relative to breast glandular tissue
- T2: hyperintense to breast glandular tissue, but less bright than cysts
- T1 C+
- rapid early enhancement
- absolute enhancement rate may be somewhat less than DCIS
- may be a homogeneous or heterogeneous pattern
- may show peripheral ("rim-like") hyperenhancement on delayed images
- dynamic enhancement pattern non-specific; all 3 types of kinetics (persistent, plateau, and washout) have been described
- rapid early enhancement
- DWI/ADC: restrict diffusion (high DWI, low ADC values)
Nuclear Medicine
PET-CT
- may be associated with mildly increased (less than liver) FDG-avidity
- at least one report of markedly increased (SUV 10-12) avidity in a papilloma with strong expression of GLUT-1transporter
Treatment and prognosis
Most centers treat solitary intraductal papillomas with surgical excision, even after benign biopsy, to exclude components of atypia or neoplasia. However, there is some controversy surrounding this, with some groups suggesting that clinical follow-up is sufficient if there is no atypia (including ADH) on core biopsy .
Given the increased risk of malignancy over a woman's lifetime when this lesion is diagnosed, compliance with screening recommendations for such patients is strongly advisable.
According to a consensus committee of the College of American Pathologists, women with this lesion have a relative risk of 1.5-2 times for developing invasive breast carcinoma in their lifetime.
Differential diagnosis
The differential includes other solid tumors that can occur in the large ducts, specifically:
- ductal carcinoma in situ
- invasive ductal carcinoma with an in situ component
- papillary carcinoma of the breast can mimic an intraductal papilloma (particularly on ultrasound)
For ultrasound appearances also consider:
- inspissated secretions within a dilated duct may mimic papillomas but have no associated vascularity
- complex breast abscess with debris: solid component mobile
- fat necrosis: also no Doppler vascularity
Siehe auch:
- duktales in situ Karzinom der Mamma
- papilläre Neoplasien der Mamma
- papilläres Mammakarzinom
- Abszess der Mamma
- intraduktale papilläre Neoplasien der Mamma
- Liponekrose
- sklerosierendes intraduktales Papillom der Mamma
und weiter:

 Assoziationen und Differentialdiagnosen zu intraductales Papillom der Mamma:
Assoziationen und Differentialdiagnosen zu intraductales Papillom der Mamma: