Bisphosphonattherapie assoziierte Femurfrakturen













Atypical femoral fractures, also known as bisphosphonate-related proximal femoral fractures, are an example of insufficiency fractures, although the direct causative link remains somewhat controversial. The atypical fracture pattern occurs in the femur shaft and may be unilateral or bilateral.
Atypical femoral fractures have been defined by the American Society for Bone and Mineral Research by the following criteria :
- location in the femoral diaphysis: distal to the lesser trochanter but proximal to the supracondylar flare
- four of five following major features
- no or minimal trauma
- mainly transverse; medially may be oblique
- must involve the lateral cortex; medially may have "medial spike"
- no or minimal comminution
- endosteal or periosteal thickening
- minor features
- generalized diaphyseal thickening
- bilaterality
- prodromal symptoms (e.g. groin pain)
- delayed healing
- exclusion criteria
- not be spiral or comminuted
- not be femoral neck or intertrochanteric
- no evidence of malignant bone tumor (primary or metastatic) or other bone diseases (e.g. Paget disease, fibrous dysplasia)
- not be periprosthetic
Epidemiology
The rate of this fracture pattern outlined above in women who are treated continuously with bisphosphonates is 1 in 1000 compared to 0.02 in 1000 for untreated women . They occur in older, postmenopausal women.
Overall, the risk for all types (i.e. both typical and atypical) of femoral fractures is lower in women who take bisphosphonates.
Clinical presentation
Most patients have been on long-term bisphosphonate therapy (> 3-5 years) and report a weeks-to-months history of thigh or groin pain . Fractures can be atraumatic or result from a low-energy mechanism (e.g. fall from standing height). They are often bilateral; in case of an atypical femoral fracture, the opposite femur should also be imaged.
Pathology
Biphosphonate and RANKL inhibitors such as denosumab are linked to this type of fracture but it has not been unquestionably proven due to a lack of high-quality data.
The proposed theory is that prolonged bisphosphonate use decreases osteoclast activity and inhibits bone remodeling, leading to microdamage that would normally be repaired but is inhibited, thus increasing skeletal fragility.
Radiographic features
Plain radiograph
- changes first occur within the lateral cortex of the proximal femur with focal periosteal reaction, cortical thickening and other changes of insufficiency fractures
- incomplete fractures affect the lateral cortex only
- if untreated, the fracture propagates medially and can progress to a complete one
- complete fractures are typically transverse, sometimes oblique (<30 degrees), and can have a 'beaked' appearance of one cortex
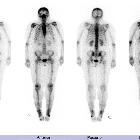
Nuclear medicine
- increased osteoblastic activity (i.e. uptake) in the lateral proximal femur on Tc-99m bone scan
MRI
MRI is useful in cases when x-ray is negative. Early changes will follow the pattern of insufficiency fractures with the lateral periosteum and cortex being initially affected .
Fractures have the following pattern:
- T1: low signal fracture line; diffuse low marrow signal
- T2 and STIR: low signal fracture line; diffuse high marrow signal
Treatment and prognosis
After a diagnosis of an atypical fracture is confirmed (complete or incomplete), antiresorptive treatment should be stopped.
Operative treatment is recommended for all patients with atypical femoral fractures. Intramedullary nailing is the preferred treatment as they are weight sharing devices and promote healing with callus in comparison to plate and screw constructs.
Delayed fracture healing occurs in ~25% of cases . Healing of atypical fractures and restoration of bone quality can be aided by teriparatide, a recombinant human parathyroid hormone (rhPTH).
Patients who present with pain and have early stress reactions (cortical thickening and peaking of the femur) are also often considered for prophylactic operative treatment.
All patients who present with atypical femoral fractures should have their contralateral femurs imaged with plain radiographs to evaluate for early changes of impending fracture, in which case prophylactic fixation is recommended.
Related pathology
Siehe auch:

 Assoziationen und Differentialdiagnosen zu Bisphosphonattherapie assoziierte Femurfrakturen:
Assoziationen und Differentialdiagnosen zu Bisphosphonattherapie assoziierte Femurfrakturen:




