haemorrhagic ovarian cyst




Hemorrhagic ovarian cysts (HOCs) usually result from hemorrhage into a corpus luteum or other functional cyst. Radiographic features are variable depending on the age of the hemorrhage. They typically resolve within eight weeks.
Clinical presentation
Patients may present with sudden-onset pelvic pain, pelvic mass, or they may be asymptomatic and the hemorrhagic ovarian cyst is an incidental finding . A hemorrhagic or a ruptured ovarian cyst is the most common cause of acute pelvic pain in an afebrile, premenopausal woman presenting to the emergency room . They can occur during pregnancy.
Pathology
Hemorrhagic ovarian cysts typically develop as a result of ovulation. Secondary to a hormone response the stromal cells surrounding a maturing Graafian follicle become more vascular, and after the oocyte has been expelled, the Graafian follicle develops into a corpus luteum with a highly vascular and fragile granulosa layer, which ruptures easily, forming a hemorrhagic ovarian cyst .
Radiographic features
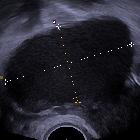
Ultrasound
Hemorrhagic ovarian cysts can have a variety of appearances depending on the stage of evolution of the blood products and clot.
- lace-like reticular echoes or an intracystic solid clot
- a fluid-fluid level is possible.
- thin wall
- clot may adhere to the cyst wall mimicking a nodule, but has no blood flow on Doppler imaging
- retracting clot may have sharp or concave borders, mural nodularity does not
- posterior acoustic enhancement
- may be less noticeable if harmonics or compounding is used
- there should not be any internal blood flow
- circumferential blood flow in the cyst wall is typical
If there is rupture of a hemorrhagic cyst, other findings may be present.
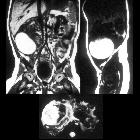
MRI
Relatively well defined cystic lesion in association with the ovary. Signal characteristics can vary depending on the age of the hemorrhage.
- T1: high signal
- T2: high signal
- "T2 shading" is suggestive of chronic blood products and is more typical of endometrioma
- hemorrhage evolves from the center of the cyst and then extends peripherally (i.e. the center may show chronic stage of hemorrhage while the periphery is more subacute)
- T1 C+ (Gd): no enhancement
Treatment and prognosis
Most hemorrhagic cysts resolve completely within two menstrual cycles (8 weeks).
Cysts with a typical appearance of a hemorrhagic cyst should lead to follow-up ultrasound or MRI imaging in 6-12 weeks if:
- the cyst is > 5 cm in diameter if the patient is pre-menopausal
or - any size of a hemorrhagic cyst if the patient is perimenopausal
In the postmenopausal patient, surgical evaluation is warranted.
A cystic structure that does not convincingly satisfy the criteria for a benign cyst cannot be considered a cyst and should be evaluated with a short interval follow-up ultrasound or MRI
Differential diagnosis
Differential considerations on ultrasound include:
- cystic ovarian neoplasm: the most helpful feature in distinguishing ovarian neoplasms from hemorrhagic cysts are
- papillary projections
- nodular septae
- color Doppler flow in the cystic structure
- endometrioma
- typically contains uniform low-level internal echoes with a hypervascular wall on Doppler ultrasound.
- more often multiple
- on MRI, endometrioma shows high signal in T1 and low signal in T2 (shading sign), although there is overlap in appearance with hemorrhagic cysts
See also
Siehe auch:
und weiter:

 Assoziationen und Differentialdiagnosen zu eingeblutete Ovarialzyste:
Assoziationen und Differentialdiagnosen zu eingeblutete Ovarialzyste: