papillary breast cancer
Papillary carcinoma of the breast is a rare ductal breast malignancy.
Epidemiology
They are thought to account for 1-2% of breast carcinomas . They typically present in postmenopausal patients with the mean age at being ~63-67 years.
Clinical presentation
A papillary carcinoma may manifest clinically as a palpable mass or nipple discharge, with the latter present in 22-34% of patients
Pathology
Papillary carcinomas may be solitary or multiple. When the epithelium of a papillary carcinoma has features diagnostic of intraductal carcinoma, the lesion is classified as papillary ductal carcinoma in situ. If a cystic component is present, the tumor is described as an intracystic papillary carcinoma (ICPC). In the absence of an appreciable cyst, a diagnosis of solid papillary carcinoma is appropriate. Invasive elements arising in a papillary carcinoma are almost always detected at the periphery of the lesion. Papillary carcinomas are usually well circumscribed and often contain hemorrhagic and cystic areas.
Histologically it is characterized by a frondlike growth pattern on a fibrovascular core lacking a myoepithelial layer.
Pathologically, four potential cellular patterns exist:
- cribriform
- compact columnar epithelial
- stratified spindle cell
- transitional form: similar to urothelial tumors
Combinations of these patterns may be seen.
Location
Approximately 50% of papillary carcinomas arise in the retro-areolar/subareolar region of the breast.
Radiographic features
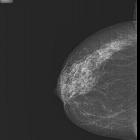
Mammography
The most common mammographic pattern of invasive papillary carcinoma is a round, oval or lobulated mass. The mass margins are usually circumscribed but may be obscured or indistinct. Accompanying microcalcifications or a dilated ductal pattern may also be present.
Breast ultrasound
Sonographic evaluation of invasive papillary carcinomas may reveal a hypoechoic and solid mass, often with posterior acoustic enhancement; alternatively, complex cystic and solid masses may be evident.
As they are relatively vascular, there are often color flow components on Doppler interrogation.
There is overlap in the imaging patterns of invasive papillary carcinoma and papillary ductal carcinoma in situ.
Galactography: ductography
For patients presenting with nipple discharge, galactography may be helpful. Like intraductal papillomas, papillary carcinomas may be evident as ductal obstruction, filling defects, or focal or diffuse ductal wall irregularity.
Breast MRI
In the case of an intracystic papillary carcinoma, it usually appears as a round or oval mass with well-defined margins. The internal composition is typically heterogeneous, with multiple nodular masses of intermediate signal intensity projecting from the periphery into the lumen. The signal intensity also dependent on the intracystic fluid composition:
- If serous, it will have low signal intensity on T1-weighted images and high signal intensity on T2-weighted images
- if there are hemorrhagic contents, it will be hyperintense on both T1- and T2-weighted images and fluid-fluid levels may be seen on T2-weighted images.
Intracystic hemorrhage is a characteristic common finding at pathologic examination of papillary carcinomas.
Contrast-enhanced MR imaging may show marked enhancement of the cyst walls, septa, and mural nodules .
Treatment and prognosis
The overall prognosis is better than for commoner types of breast malignancy such as invasive ductal carcinoma not otherwise specified (NOS).
Siehe auch:
- intraductales Papillom der Mamma
- papilläre Neoplasien der Mamma
- Neoplasien der Mamma
- intraduktale papilläre Neoplasien der Mamma
- intracystic papillary carcinoma of the breast
und weiter:

 Assoziationen und Differentialdiagnosen zu papilläres Mammakarzinom:
Assoziationen und Differentialdiagnosen zu papilläres Mammakarzinom: