Primary intraosseous hemangioma

























Primary intraosseous hemangiomas are vascular hamartomas arising within bone, seen most frequently in the vertebrae or skull. Given their nonneoplastic nature, some authors prefer to refer to these lesions as vascular malformations rather than hemangiomas. These come in four histological varieties (see below) .
Epidemiology
Intraosseous hemangiomas are common, with vertebral hemangiomas seen in 10-15% of the adult population. They are more commonly encountered in men (M:F ratio of 2:1) and typically seen in the 4 to 5 decade of life.
Clinical presentation
These tumors are slow growing and are generally asymptomatic unless they exert mass effect on sensitive structures. Occasionally they may present as a swelling or a palpable mass, especially in the skull. When large and strategically located, they may present with a pathological fracture.
If they are high-flow lesions, shunt-related symptoms may also be present.
Pathology
Primary intraosseous hemangiomas are slow growing vascular malformations, usually located in the medullary cavity. They are classified as benign, but rarely may be locally aggressive.
Histological subtypes
Intraosseous hemangiomas come in four histologic types:
Histologically, intraosseous hemangiomas demonstrate hamartomatous vascular tissue within endothelium, but may also contain fat, smooth muscle, fibrous tissue, and thrombi.
It should be noted that it is difficult to distinguish between the various histological types on imaging, except for those with a large arterial component.
Location-specific subtypes
- vertebral hemangioma
- sacral hemangioma
- skull vault hemangioma
- intracortical hemangioma
Radiographic features
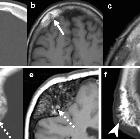
Plain radiograph
Plain radiographs are usually the first line of imaging and may be sufficient in vertebral or calvarial lesions. Findings include:
- prominent trabecular pattern
- sclerotic vertebra with vertical trabeculae: corduroy sign
- lytic calvarial lesions with spoke-wheel appearance
- irregular and lytic in long bones, with a honeycomb appearance
CT
Usually as an incidental finding, especially in the vertebrae.
Better visualization of thickened vertical trabeculation: polka-dot appearance on axial images and corduroy sign on coronal and sagittal images.
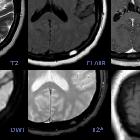
MRI
Signal intensity is somewhat variable, depending largely on the amount of fat content.
- T1
- high is more common (fat rich)
- intermediate to low signal intensity is seen in fat poor hemangiomas
- T2: high
- T1 C+ (Gd): enhancement is often present
- STIR: intermediate or high
MRI is the ideal modality to demonstrate mass-effect complications, such as neural impingement and extraosseous extension.
Nuclear medicine bone scan
Usually normal but may show increased or decreased uptake.
Treatment and prognosis
Treatment is reserved for symptomatic lesions, and a number of options exist:
- radiation therapy
- embolization to reduce intraoperative blood loss
- surgical resection, especially if complicated by spinal cord compression
- vertebroplasty
- intralesional ethanol injection
Siehe auch:
- Hämangiom Schädelkalotte
- Hämangiom der Wirbelsäule
- pathologische Fraktur
- Hämangiom
- Vertebroplastie
- multiple T2 hyperintense ossäre Läsionen
- Corduroy-Zeichen (Wirbelkörperhämangiom)
- epitheloides Hämangiom des Knochens
und weiter:

 Assoziationen und Differentialdiagnosen zu intraossäres Hämangiom:
Assoziationen und Differentialdiagnosen zu intraossäres Hämangiom: