Hämangiom Schädelkalotte


























Skull vault hemangiomas (SVH), or hemangiomas of the calvaria, are benign slow-growing vascular lesions affecting the skull diploe in any location. They have been more recently renamed osseous venous (low-flow) vascular malformations given their nonneoplastic nature, but "hemangioma" remains commonly used.
Please refer to the article on intraosseous hemangiomas for a general discussion of that entity.
Epidemiology
The calvaria is the second most prevalent site for intraosseous hemangiomas, particularly the frontal and parietal bones . It represents 10% of benign neoplasms of the skull and 0.2% of all osseous tumors . Commonly occurs in women in the 4-5decades of life with a 3:1 female-male ratio .
Clinical presentation
These tumors are slow-growing and are generally asymptomatic, unless when palpable due to a lump produced by an expansion of the outer table .
Pathology
As an intraosseous hemangioma, skull vault hemangiomas are classified as venous, cavernous, or capillary type, according to their predominant vascular network. Histologically, it demonstrates hamartomatous vascular tissue within endothelium, but may also contain fat, smooth muscle, fibrous tissue, and thrombus .
Radiographic features
Plain radiograph
Lytic lesion with a sclerotic rim (usually with a honeycomb- or sunburst-like appearance).
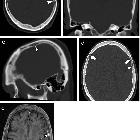
CT
Usually presents as an expansile bone lesion with thin borders and a characteristic sunburst pattern of trabecular thickening radiating from a common center . Erosions of both internal or external plates can occur and may be associated with internal or external tumor expansion. Sometimes, bony trabeculae can grow beyond the cortical bone, and simulate an aggressive pseudo-"hair-on-end" periosteal reaction .
Angiography (DSA)
DSA is important for the surgical planning of smaller lesions and embolization of larger ones.
MRI
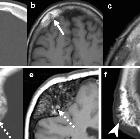
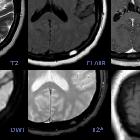
Signal intensity is somewhat variable, depending largely on the amount of fat content .
- T1: typically hyperintense, though atypical T1 hypointense forms are not rare.
- T2/FLAIR: hyperintense signal with a "bunch of grapes" appearance
- T1 C+ (Gd): homogeneous enhancement is often present
Treatment and prognosis
Treatment usually not necessary. Rare indications include: mass effect, hemorrhage control, and aesthetic improvement. Treatment options are:
- radiation therapy
- embolization to reduce intraoperative blood loss
- surgical resection
- intralesional ethanol injection
Siehe auch:
- Läsionen der Schädelkalotte
- Osteolysen der Kalotte
- Sinus pericranii
- intraossäres Hämangiom
- venöse Kanäle und Lakunen der Kalotte
und weiter:

 Assoziationen und Differentialdiagnosen zu Hämangiom Schädelkalotte:
Assoziationen und Differentialdiagnosen zu Hämangiom Schädelkalotte: