tracheobronchopathia osteochondroplastica










Tracheobronchopathia osteochondroplastica (TO) is a very rare idiopathic non-neoplastic tracheobronchial abnormality.
Epidemiology
The estimated prevalence on routine bronchoscopy can be up to 0.7%. It typically affects those in the 5 to 6 decades and there may be a male predilection .
Clinical presentation
Most patients are asymptomatic. Those who have symptoms may present with cough, shortness of breath on exertion, wheezing or recurrent respiratory infection. Hemoptysis can occasionally result from an ulceration of a nodule or an acute infection.
Pathology
There is development of osseous or cartilaginous 1-8 mm nodules or both in the submucosa of the trachea and bronchial walls. They may be either focal or diffuse. There is characteristic sparing of the posterior membranous portion of the trachea .
There are two possible theories of pathogenesis :
- ecchondrosis and exostosis from cartilage rings
- cartilaginous and osseous metaplasia of the elastic tissue in the internal elastic fibrous membrane
Location
- classically affects the lower two-thirds of the trachea and proximal portions of the bronchi
- only affects the anterior and lateral walls of trachea
Radiographic features
Plain radiograph
Chest radiograph may show irregularity and narrowing of typically affected segments of trachea and bronchi.
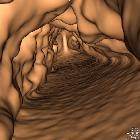
CT
- irregular thickening and nodularity of tracheal cartilage, sparing the posterior (membranous) tracheal wall
- small discrete endophytic nodules (typically ~3-8 mm) may be cartilagenous or calcific (ossified)
- larger nodules may result in luminal narrowing, and should be specifically reported by location and degree of airway narrowing
- diffuse airway narrowing is not typical
- overall appearance is much more irregular compared to benign cartilage calcification
Treatment and prognosis
It is a benign condition and often no intervention is required in asymptomatic cases. Successful recovery with NSAIDS and dapsone have been reported in symptomatic cases. Overall prognosis is generally good and is dependent upon airway stenosis caused by nodules.
History and etymology
Initially described in 1857 by Samuel Wilks (1824-1911), as "ossific deposits in the larynx, trachea and bronchi" in a 38-year-old-male who died of pulmonary tuberculosis . The condition was later termed "tracheopathia osteochondroplastica" in 1910 by German pathologist Karl Ludwig Aschoff (1866-1942) .
Differential diagnosis
Imaging differential considerations include:
- tracheobronchial amyloidosis
- unlike TO, classically circumferential involvement
- may appear as focal or diffuse narrowing
- relapsing polychondritis
- like TO, spares posterior membranous tracheal wall
- more likely smooth, hyperdense mural thickening
- patients usually have other clinical findings of cartilaginous inflammation
Siehe auch:
- Granulomatose mit Polyangiitis
- Rezidivierende Polychondritis
- tracheobronchiale Papillomatose
- diffuse Trachealverengung
- Amyloidose des Tracheobronchialsystem
- Trachealverkalkungen
und weiter:

 Assoziationen und Differentialdiagnosen zu Tracheobronchopathica osteochondroplastica (TBO):
Assoziationen und Differentialdiagnosen zu Tracheobronchopathica osteochondroplastica (TBO):




