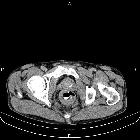
rectal carcinoma


































Rectal cancers, although sharing many of the features of generic colorectal carcinoma (CRC), has different preoperative imaging assessment, with MRI rectum as the mainstay for local staging, and distinct surgical techniques (i.e. total mesorectal excision).
Epidemiology
Rectal cancer is generally considered a disease of the elderly, but the incidence of cases in patients under the age of 50 has been increasing. There is a slight male predilection, not seen in cancers of the rest of the large bowel.
Clinical presentation
Patients often present with altered bowel habit or rectal bleeding .
Pathology
Similarly to the rest of the colon, the vast majority of rectal tumors are adenocarcinomas (98%), with carcinoid tumors, lymphoma, and GIST making up most of the remainder .
Radiographic features
Although CT can make the diagnosis in more advanced cases, due to better soft-tissue contrast, MRI has become the fundamental imaging modality for evaluation and staging. Endorectal ultrasound also has a role in the staging, particularly for assessment and differentiation between T1 and T2 disease, but is not commonly performed by a radiologist.
MRI may be performed for:
- diagnosis and/or locoregional staging
- helps evaluate which patients may benefit from neoadjuvant therapy (usually stage II and III) and for evaluating poor prognostic factors
- helps surgical planning
- assessment of the effectiveness/response of neoadjuvant therapy
- monitoring for recurrence post-therapy
MRI
MRI is able not only to assess tumor stage but other important prognostic features such as extramural venous invasion (EMVI), tumor deposits and lymph node metastases. The key sequences are T2-weighted images parallel and perpendicular to the axis of the segment of the rectum containing the tumor. For more information, see MRI protocol for assessment of rectal cancer.
Factors to be assessed and described on MRI report:
- morphology of primary tumor: annular/ulcerating/polypoidal/villous/eroding/mucinous/signet cannot be assessed
- invading edge of tumor (e.g. x o'clock to y o'clock)
- distance of distal edge from the anal verge
- distance of distal edge from puborectalis sling
- longitudinal extent
- whether it lies above or below peritoneal reflection with approximate measurement
- T stage
- whether it is confined to or extends through muscularis propria
- extent of extramural spread (T3 disease) and whether peritoneum (T4a) or other organs (T4b) are invaded
- distance from the mesorectal fascia
- extramural venous invasion (EMVI)
- presence of tumor deposits
- N (locoregional) stage
- size is not a reliable indicator of nodal involvement
- irregular or spiculated margin and heterogeneous signal intensity
- number of nodes
- closest node to the mesorectal fascia
- pelvic sidewall nodes: none/benign-looking/malignant-looking
- evidence of peritoneal nodal involvement
Please refer to the article on Rectal cancer (staging) for further details on how to apply and report the TNM staging on imaging.
Treatment and prognosis
The mainstay of treatment is surgical excision, however preoperative down-staging with either radiotherapy alone (more common in Europe) or combined chemo-radiotherapy (more common in the US) is employed in T3 and/or N1 disease (see rectal cancer staging) .
Depending on the stage at the time of resection local recurrence rates vary from 3-32% with overall good 5-year survival in T1 and T2 tumors (85-100% and 70% respectively) . Some focal T1 lesions are candidates for transanal endoscopic microsurgery.
The majority of local recurrences occur within 20-36 months , have positive resection margins, and have a major impact on prognosis, with 80-90% of these patients succumbing to the disease within 5 years .
Some authors suggest that a circumferential resection margin (CRM) of less than 1 or 2 mm (the exact cut-off is debated) confers a poorer prognosis and patients should be considered for neoadjuvant treatment .
See also
Siehe auch:
- Karzinoid
- Kolorektales Karzinom
- Kolon
- Gastrointestinaler Stromatumor
- präoperatives Staging Rektumkarzinom
- MRT Rektumkarzinom
- circumferential resection margin (CRM) rektum
- Tumoren des Rektums
- anal sphincter complex
und weiter:
- Rektum
- freie retroperitoneale Luft
- Vaginalkarzinom
- pelvic MRI protocol : Rectal cancer
- transposed ovaries
- Rektum Ca Metastasierung
- EMVI
- rectal cancer with bone metastasis
- Metastasen in der Cervix uteri
- adenosquamous carcinoma of the rectum
- anorectal tumours
- rectal carcinoma recurrence
- colorectal carcinoma (rectosigmoid)
- rectal adenocarcinoma
- Leiomyosarkom des Rektums
- Polypen des Rektums

 Assoziationen und Differentialdiagnosen zu Rektumkarzinom:
Assoziationen und Differentialdiagnosen zu Rektumkarzinom:




