superior sagittal sinus thrombosis






Superior sagittal sinus thrombosis (SSST) is the most common type of dural venous sinus thrombosis and is potentially devastating.
This article focuses on the specific features related to the superior sagittal sinus thrombosis, please refer to the dural venous sinus thrombosis article for a general discussion.
Risk factors include pregnancy, dehydration, hypercoagulable states, pancreatitis.
Clinical presentation
As with all cerebral venous thrombosis, the presentation is highly variable, ranging from completely asymptomatic to a rapid fulminant course with cerebral hemorrhage and death. Presentation includes:
- headache: 53%, most common
- seizures: 48%
- hemi-, quadri-, or paraplegia: 48%
- visual disturbances: 25%
- nuchal rigidity: 18%
Radiographic features
Features are the same as those for other sinuses (please refer to dural venous sinus thrombosis).
CT
Unenhanced CT is usually the first imaging investigation performed given the nonspecific clinical presentation in this case. When not associated with venous hemorrhage or infarction, it can be a subtle finding on CT images, relying on hyperdensity of the sinus being identified. Potential findings include:
- cord sign
- dense vein sign
- a potential pitfall is interpreting the distal superior sagittal sinus as being hyperdense near the torcular herophili
- the walls at this location can be thick, measuring up to 2-3 mm
- cerebral edema: secondary to venous hypertension
- cortical/cerebral swelling
- unilateral or bilateral venous hemorrhage
With contrast administration, especially with a CT venogram, a filling defect in the sinus is sought. Multiplanar reformatted CT venography has been reported with a sensitivity of 95% for this diagnosis. When in the superior sagittal sinus it is referred to as the empty delta sign. Signs of contrast CT include:
- empty delta sign (is specific to the superior sagittal sinus)
- gyral enhancement
- prominent intramedullary veins
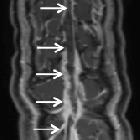
MRI
The clot acutely is isodense on T1 and hypointense on T2 (this can mimic a flow void), with subacute clot becoming hyperintense on T1. All the findings listed in the CT section are also seen on MRI. MRV will demonstrate lack of flow.
Differential diagnosis
For high attenuating cerebral veins on a non-contrast CT scan consider high hematocrit and/or hemoglobin levels.
Siehe auch:
und weiter:

 Assoziationen und Differentialdiagnosen zu Sinusthrombose Sinus sagittalis superior:
Assoziationen und Differentialdiagnosen zu Sinusthrombose Sinus sagittalis superior:



