Adenopathy
Lymph node enlargement (rarely lymphadenomegaly) is often used synonymously with lymphadenopathy, which is not strictly correct.
Terminology
Lymphadenopathy (or adenopathy) is, if anything, a broader term, referring to any pathology of lymph nodes, not necessarily resulting in increased size; this includes abnormal number of nodes, or derangement of internal architecture (e.g. cystic or necrotic nodes). In addition, increase in size is not always pathologic; some nodes are bigger than others normally (e.g compare jugulodigastric nodes to mesenteric nodes), and reactive nodes are a healthy response and do not imply pathology of the node itself.
There are approximately 600 lymph nodes, of which only some are available to direct palpation. Only some nodes (including neck, axilla and groin) should ever be palpable and these should be soft and non-tender.
Pathology
Etiology
There are many (many) causes of lymph node enlargement which include:
- infective (acute suppurative)
- reactive
- follicular hyperplasia
- paracortical hyperplasia
- sinus histiocytosis
- granulomatous
- neoplastic
- drug-induced, e.g. cyclosporin, phenytoin, methotrexate
- lipid storage diseases
- IgG4-related sclerosing disease
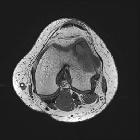
Radiographic features
The upper limit in size of a normal node varies with location, and of course the size cut-off used depends on the desired sensitivity and specificity.
Cervical lymph nodes
See the separate article: cervical lymph node metastasis (radiologic criteria).
Mediastinal lymph nodes
In general 10 mm is considered the upper limit for normal nodes (short axis diameter) . This does not, of course, take into consideration the fact that all nodal metastases must start at microscopic size, and thus using only size criteria will miss micrometastases. In the setting of lung cancer staging a sensitivity of 0.83 and a specificity of 0.82 are quoted for CT .
See the separate article: mediastinal lymph node enlargement.
Mesenteric lymph nodes
Mesenteric nodes are increasingly visualized as a result of multidetector volume acquisition and are most easily seen on coronal reformats.
Although 3 mm has previously been used as the upper limit for the short axis diameter of mesenteric lymph nodes, up to 39% of healthy normal patients have larger nodes than this. As such a figure of 5 mm is considered normal .
See the separate article: normal mesenteric lymph nodes.
See also
- differential diagnosis of high attenuation lymphadenopathy
- differential diagnosis of low attenuation lymphadenopathy
Siehe auch:
- zystische Lymphknoten
- Vergrößerung der zervikalen Lymphknoten
- Rosai-Dorfman-Erkrankung
- hyperdenser Lymphknoten
- normal mesenteric lymph nodes
und weiter:
- Milzinfarkt
- mediastinale Raumforderungen
- Tumoren des hinteren Mediastinums
- posterior mediastinal masses
- low attenuation lymphadenopathy
- Mastozytose
- Läsionen im kardiophrenischen Winkel
- Skrofeln
- Rai staging system for chronic lymphoid leukaemia
- cervical lymph node staging
- hypervaskularisierte Lymphknoten
- chronic lymphocytic leukaemia
- IgG4-assoziierte Erkrankung
- echoarme Lymphknoten
- eosinophilic hyperplastic lymphogranuloma
- tuberkulöse Otomastoiditis
- sonographic features of malignant lymph nodes
- benigne reaktive Lymphadenopathie

 Assoziationen und Differentialdiagnosen zu Adenopathy:
Assoziationen und Differentialdiagnosen zu Adenopathy: