bone infarction















Bone infarction is a term used to refer to osteonecrosis within the metaphysis or diaphysis of a bone. Necrosis is a type of cell death due to irreversible cell injury, which can be recognized microscopically by alterations in the cytoplasm (becomes eosinophilic) and in the nucleus (swelling, pyknosis, karyorrhexis, karyolysis). Bone infarction is a result of ischemia, which can lead to destruction of bony architecture, pain, and loss of function . Bone infarctions have numerous causes and have fairly distinctive imaging features on conventional radiography, CT and MRI.
Terminology
Medullary infarct is a fairly equivalent term to bone infarct but is less frequently used. The term may also be applied to some cases involving the epiphysis, but should not be used to describe subchondral osteonecrosis, in which case avascular necrosis (AVN) is preferred.
Pathology
Infarction begins when blood supply to a section of bone is interrupted. Once an infarct is established, a central necrotic core develops which is surrounded by a hyperemic ischemic zone. With time collagen granulation tissue becomes layered around the necrotic core. Demarcation between the normal surrounding marrow, the ischemic zone, and the necrotic core accounts for many of the radiographic appearances of bone infarcts.
Due to the smaller diameter of terminal vessels and the lack of collateral vascularization, convex articular surfaces are affected the most. Impairment of blood flow may be caused by vascular compression, trauma, vessel occlusion by nitrogen bubbles (caisson disease) or rigid sickle cells (sickle cell anemia). The mechanism of ischemia and necrosis in other non-traumatic osteonecroses is not yet fully understood .
Etiology
General causes of osteonecrosis include:
- trauma
- caisson disease
- hemoglobinopathies, e.g. sickle cell disease
- radiotherapy
- connective tissue disorders
- renal transplantation
- corticosteroid excess (both endogenous and exogenous)
- pancreatitis
- gout
- Gaucher disease
- alcohol
- Behçet's disease
The above list applies to both bone infarct and subchondral avascular necrosis. Some conditions are more likely to lead to one over the other: Sickle cell disease and Gaucher disease very commonly cause bone infarcts and less commonly cause subchondral AVN.
Radiographic features
General features include:
- location
- medullary
- metaphyseal
- serpiginous border
- often symmetrical and/or multiple
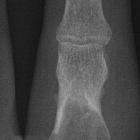
Plain radiograph
There is a significant delay between the infarct onset and development of radiographic signs. Classic description is of medullary lesion of sheet-like central lucency surrounded by shell-like sclerosis with a serpiginous border. Discrete calcification and periostitis may also be seen.
CT
Generally does not reveal much more than the plain film.
MRI
An important feature in differentiating bone infarct from other medullary lesions is that the central signal usually remains that of normal marrow. The marrow is not replaced.
- T1
- serpiginous peripheral low signal due to granulation tissue and, to a lesser extent, sclerosis
- peripheral rim may enhance post gadolinium
- central signal usually that of marrow
- T2
- acute infarct may show ill-defined non-specific area of high signal
- double-line sign: hyperintense inner ring of granulation tissue and a hypointense outer ring of sclerosis
- absence of double-line sign does not exclude bone infarct
- central signal usually that of marrow
- gradient echo
- will also show double-line
- edema obscured by susceptibility
Nuclear medicine
- bone scan
- no uptake (cold spot) where blood supply absent
- mildly increased uptake at periphery during acute phase
Treatment and prognosis
Complications
Bone infarcts may occasionally dedifferentiate to a tumor such as :
- malignant fibrous histiocytoma (most common )
- osteogenic sarcoma
- fibrosarcoma of bone
- angiosarcoma of bone (extremely rare)
This most commonly occurs around the knee .
Differential diagnosis
General imaging considerations include:
- enchondroma: chondroid matrix, central marrow signal is absent
- healing non-ossifying fibroma
- normal red marrow: will not extend beyond physeal scar
- marrow tumor: central marrow signal is absent
Siehe auch:
- nicht ossifizierendes Fibrom
- Enchondrom
- Knocheninfarkt Tibia
- Knocheninfarkt Femur
- Knocheninfarkt Humerus
- differentiation between bone infarction and enchondromas
- red marrow
und weiter:
- Aseptische Knochennekrose
- intraossäres Lipom
- Sichelzellenanämie
- Chondrom
- solitary sclerotic bone lesion
- bones
- chondroide Tumoren
- Knochenläsionen der Diaphyse
- Knochentumor Verkalkungen
- acute bone infarct due to sickle cell anemia
- humerus enchondroma
- Doppellinienzeichen Osteonekrose
- bone infarct with epiphyseal involvement

 Assoziationen und Differentialdiagnosen zu Knocheninfarkt:
Assoziationen und Differentialdiagnosen zu Knocheninfarkt: