Granulomatosis with polyangiitis (upper respiratory tract manifestations)

The upper respiratory tract manifestations of granulomatosis with polyangiitis (GPA) are common and affect most patients.
For a general discussion of the condition, please refer to the main article on granulomatosis with polyangiitis (GPA). For other organ-specific radiographic features, please refer to individual articles:
- granulomatosis with polyangiitis: pulmonary manifestations
- granulomatosis with polyangiitis: renal manifestations
- granulomatosis with polyangiitis: CNS manifestations
- granulomatosis with polyangiitis: orbital manifestations
Granulomatosis with polyangiitis (previously known as Wegener granulomatosis), is a multi-system systemic necrotizing non-caseating granulomatous vasculitis affecting small to medium-sized arteries, capillaries and veins.
Epidemiology
A rare disease predominantly affecting individuals in the 5 to 7 decades of life, with a slight predilection towards males.
Clinical presentation
The majority of patients of GPA have upper respiratory tract involvement, most commonly presenting with nasal obstruction, rhinitis and epistaxis - akin to chronic rhinosinusitis. Often presents following a protracted period of symptoms (months to years), due to being mistaken for chronic sinusitis clinically.
Pathology
GPA manifests in the upper respiratory tract with :
- sinusitis/mastoiditis/otitis
- sclerosing osteitis of the nasal cavity
- sinonasal mucosal ulcers
- bone deformities, e.g. nasal septal perforation, nasal saddle deformity
- subglottic stenosis
Radiographic features
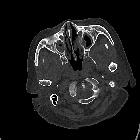
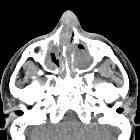
CT
- non-contrast CT
- sinonasal mucosal thickening +/- air-fluid levels +/- soft tissue nodules
- bony/cartilaginous erosions, in particular, affecting lamina papyracea, nasal septum, and lateral nasal cavity wall +/- perforation
- post-contrast CT
- enhancing soft tissue nodules
MRI
- T1: low-to-intermediate signal intensity nodules or mass-like mucosal lesions
- T1 C+ (Gd): enhancement of involved mucosal tissue
- T2: low signal intensity of nodules, relative to inflamed (edematous) surrounding mucosa
Treatment and prognosis
Usually consists of a combination of corticosteroids and cytotoxic agents such as cyclophosphamide. Generally indolent, but if the fulminant disease occurs with secondary sepsis, antibiotics are required.
Differential diagnosis
Possible considerations include:
- sinusitis
- chronic sinusitis
- fungal sinusitis
- sinonasal polyposis
- sinonasal sarcoidosis
- nasal necrosis due to cocaine
- other causes of nasal septal perforation
Siehe auch:

 Assoziationen und Differentialdiagnosen zu Granulomatose mit Polyangiitis Manifestationen oberer Respirationstrakt:
Assoziationen und Differentialdiagnosen zu Granulomatose mit Polyangiitis Manifestationen oberer Respirationstrakt:
