granulomatosis with polyangiitis


















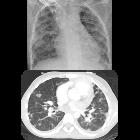
Granulomatosis with polyangiitis (GPA), previously known as Wegener granulomatosis, is a multisystem necrotizing non-caseating granulomatous c-ANCA positive vasculitis affecting small to medium-sized arteries, capillaries, and veins, with a predilection for the respiratory system and kidneys.
This article discusses GPA in general. For organ-specific radiographic features, please refer to individual articles:
- granulomatosis with polyangiitis: pulmonary manifestations
- granulomatosis with polyangiitis: renal manifestations
- granulomatosis with polyangiitis: upper respiratory tract manifestations
- granulomatosis with polyangiitis: CNS manifestations
- granulomatosis with polyangiitis: orbital manifestations
Epidemiology
There is a slight male predilection and onset is typically at approximately 50 years of age .
Clinical presentation
Presentation depends on which organ systems are involved:
- cough and hemoptysis
- subacute to chronic history of nasal obstruction, rhinitis, and epistaxis
- proteinuria and hematuria
Symptoms related to other organ systems are less frequent, due to a corresponding infrequency of involvement (musculoskeletal symptoms, ocular symptoms, skin changes) .
Systemic symptoms such as anorexia, malaise and fever are also common .
Diagnostic criteria
The 1990 American College of Rheumatology criteria requires at least two of the four listed below (sensitivity 88.2% and specificity 92%)
- positive biopsy for granulomatous vasculitis
- urinary sediment with red blood cells
- abnormal chest radiograph
- oral or nasal inflammation
Pathology
It results from an immune-mediated vascular injury.
Histology
Histologically necrotizing granulomas with an associated vasculitis are the dominant feature.
Markers
In 90% of cases, cANCA (PR3) is positive and the levels correlate with disease activity .
Classification
The classic triad of organ involvement consists of:
- lungs: involved in 95% of cases
- upper respiratory tract / sinuses: 75-90%
- kidneys: 80%
In terms of extent, granulomatosis with polyangiitis can be classified as:
- classical: full triad
- limited: not having the full triad
- usually respiratory tract involvement only
- renal only involvement has been described but is uncommon
- widespread: additional organ involvement
- skin (50%)
- eyes (45%)
- peripheral nervous system (35%)
- occasionally also other organs, such as the heart and gastrointestinal tract
Treatment and prognosis
Treatment is typically with cyclophosphamide, methotrexate and/or steroids. More recently agents such as Rituximab are also used.
Without treatment, granulomatosis with polyangiitis is rapidly progressive with death usually occurring within a year of diagnosis, with only 10% of patients surviving 2 years . Appropriate medical therapy has dramatically increased long term survival .
History and etymology
The former name "Wegener granulomatosis" comes from the German pathologist Friedrich Wegener who first described it in 1936 . Wegener was a member of the Nazi party and it is suspected that he took part in experiments on concentration camp inmates. Following the discovery of his past history, the current name "granulomatosis with polyangiitis" has been proposed .
Differential diagnosis
General imaging differential considerations include:
- eosinophilic granulomatosis with polyangiitis (EGPA)
- lymphomatoid granulomatosis
- sarcoidosis
- microscopic polyangiitis
Siehe auch:
- Sarkoidose
- Churg-Strauss-Syndrom
- septische Embolie Lunge
- Kavernöse Lungenläsionen
- pulmonale Vaskulitis
- lymphomatoid granulomatosis
- Granulomatose mit Polyangiitis Manifestationen in der Lunge
- granulomatosis with polyangiitis pulmonary manifestations
- Granulomatose mit Polyangiitis zerebrale Manifestationen
- granulomatosis with polyangiitis splenic manifestations
- granulomatosis with polyangiitis upper respiratory tract manifestations
- granulomatosis with polyangiitis renal manifestations
und weiter:
- Langerhanszell-Histiozytose der Lunge
- Vaskulitis
- Lungenabszess
- umgekehrtes Halozeichen Lunge
- Ileitis terminalis
- reverse halo sign
- inflammatorischer Pseudotumor der Orbita
- Milchglasverschattungen
- Aortitis
- Tumoren der Nasennebenhöhlen
- Metastasen in der Orbita
- Epistaxis
- Pneumocystis jiroveci Pneumonie
- causes of pulmonary arterial hypertension
- kavernisierende Lungenmetastasen
- pulmonary cavity (mnemonic)
- differential of chronic alveolar opacities
- Mikroskopische Polyangiitis
- adult chest radiograph common exam pathology
- chronische abakterielle Mastitis
- Sigmaperforation
- PLCH
- chronic bilateral airspace opacification
- diffuse Trachealwandverdickung
- Tracheobronchopathica osteochondroplastica (TBO)
- Rheuma Differentialdiagnose
- Nasenseptumdefekt
- hypertrophe Pachymeningitis
- tracheobronchiale Papillomatose
- diffuse Alveolarblutung
- Hämoptyse
- zystische Lungenmetastasen
- diffuse Trachealverengung
- pulmonary manifestations of lymphomatoid granulomatosis
- Kutane leukozytoklastische Angiitis
- juvenile laryngotracheal papillomatosis
- idiopathische granulomatöse Mastitis
- diffuse Lungenblutung
- angiocentric immunoproliferative lesion
- Halozeichen Lunge
- diffuse pulmonary hemorrhage as the initial manifestation of Wegener granulomatosis
- granulomatöse Mastitiden allgemein
- pulmonary Wegener’s granulomatosis with splenic involvement
- segmentale arterielle Mediolyse (SAM)
- tracheobronchiale Chondritis
- Morbus Wegener Milz
- wegener granulomatosis thoracic
- Kaverne der Lunge
- Knorpelentzündung
- Merkspruch Nasenseptumperforation
- Granulomatose mit Polyangiitis renale Manifestationen
- Granulomatose mit Polyangiitis Manifestationen oberer Respirationstrakt
- granulomatöse Arteriitis
- pulmonary wegeners granulomatosis
- Vaskulitis im Gastrointestinaltrakt
- sinonasale Erkrankungen
- chronische Periaortitis

 Assoziationen und Differentialdiagnosen zu Granulomatose mit Polyangiitis:
Assoziationen und Differentialdiagnosen zu Granulomatose mit Polyangiitis: