osteofibrous dysplasia









 nicht verwechseln mit: Fibröse Dysplasie
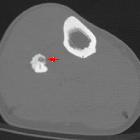
nicht verwechseln mit: Fibröse DysplasieOsteofibrous dysplasia is a benign fibro-osseous cortical lesion that occurs almost exclusively in the tibia and fibula. It is most commonly seen in the mid-diaphysis of the tibia. Some consider it synonymous with ossifying fibroma because of histological similarities, but it is generally considered a separate entity due to different presentation and treatment.
Terminology
A commonly used synonym is ossifying fibroma of the long bones.
Epidemiology
- most common in younger patients, e.g. ~ 10 years of age
- less commonly reported in older patients, up to 63 years of age
- slight male predilection (3:2 ratio )
Clinical presentation
Most patients present with pain and swelling, and patients may present secondary to a pathological fracture.
Pathology
Osteofibrous dysplasia is considered as a benign, non-neoplastic condition. Some consider it as part of a spectrum of osteofibrous dysplasia-like adamantinoma and adamantinoma.
Microscopic appearance
Histology shows trabecular bone woven within fibrous stroma with osteoblastic rimming and mature lamellar bone.
It is closely related to fibrous dysplasia (fibrous dysplasia is predominantly medullary), but the zonal phenomenon and osteoblastic rimming of bony trabeculae are absent in fibrous dysplasia.
Osteofibrous dysplasia and ossifying fibroma of the jaw have similar histological characteristics, but osteofibrous dysplasia shows cytokeratin-positive cells, whereas ossifying fibroma of the jaw shows psammomatous calcification, which are exclusive features.
Although adamantinoma can contain osteofibrous dysplasia-like components, nests or strands of an epithelioid cell are the differentiating feature between adamantinoma and osteofibrous dysplasia.
Adamantinoma with scarce epithelioid component and mostly composed of osteofibrous dysplasia-like tissue are considered as osteofibrous dysplasia-like adamantinoma.
Radiographic features
Osteofibrous dysplasia is classically a lytic lesion centered in the tibial cortex, often with sclerotic margins. Because of its similarity to adamantinoma, a much more aggressive pathology, a primary issue is differentiating between the two.
Due to intralesional heterogeneity, needle biopsy may result in diagnostic misclassification, particularly with underestimation of aggressive lesions. Thus, radiologic-pathologic correlation is important with benign or equivocal biopsy results .
Osteofibrous dysplasia tends to be:
- smaller (mean 6-7 cm versus 10-17 cm for adamantinoma)
- with more distinct margins
- less likely to involve the medullary cavity
Plain radiograph
Plain radiograph remains the initial and chief investigation.
- location:
- along long axis: mid-diaphysis, especially anteriorly
- along transverse axis: cortical with medullary encroachment
- consistency
- lucent or ground-glass
- lobular-to-bubbly in appearance
- margins
- narrow zone of transition
- sclerosis common
- no nidus
- no aggressive periosteal reaction
- benign-appearing periosteal reaction is non-specific, and can be seen in all lesions along the osteofibrous dysplasia/adamantinoma spectrum
- +/- pseudotrabeculation and anterior bowing
MRI
MRI is helpful in evaluation of suspected osteofibrous dysplasia, particularly to evaluate the extent of intramedullary involvement. Complete medullary cavity involvement is more suggestive of adamantinoma.
- T1: intermediate signal
- T2: intermediate-to-high signal
- T1C+: diffuse and intense enhancement.
- +/- soft tissue component (non-specific)
- can be seen in all lesions along the osteofibrous dysplasia/adamantinoma spectrum
- no aggressive cortical destruction
Treatment and prognosis
Surgery is reserved for lesions that are large or demonstrate aggressive behavior.
They usually have an excellent prognosis and usually, stabilize or spontaneously regress once the child is over 10 years old.
It can be locally destructive and may result in pathological fracture, subsequently pseudarthrosis.
Local recurrences can occur after surgery with some aggressive recurrence, possibly due to components of adamantinoma or possible transformation to adamantinoma.
Differential diagnosis
Consider
- ossifying fibroma
- adamantinoma
- osteofibrous dysplasia-like adamantinoma
- intracortical fibrous dysplasia
Siehe auch:
- Osteoid-Osteom
- Fibröse Dysplasie
- nicht ossifizierendes Fibrom
- Kryptorchismus
- Ossifizierendes Fibrom
- Adamantinom der langen Röhrenknochen
- Admantinom mit dem Bild einer osteofibrösen Dysplasie
und weiter:

 Assoziationen und Differentialdiagnosen zu Jaffé-Campanacci-Syndrom:
Assoziationen und Differentialdiagnosen zu Jaffé-Campanacci-Syndrom: