posterior shoulder dislocation
























Posterior shoulder dislocations are far less common than anterior shoulder dislocations and can be difficult to identify if only AP projections are obtained. A high index of suspicion is helpful.
Epidemiology
Posterior shoulder dislocations account for only 2-4% of all shoulder dislocations (the vast majority are anterior) .
Mechanism
Typically the humeral head is forced posteriorly in internal rotation while the arm is abducted . In adults, convulsive disorders are the most common cause. Electrocution is a classic but uncommon cause of posterior shoulder dislocation. In both situations, bilateral dislocations are not infrequent .
Occasionally, they can be the result of strength imbalance within the rotator cuff muscles. Posterior dislocations may even go unnoticed, especially in elderly patients .
Radiographic features
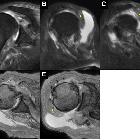
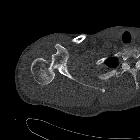
Plain film series usually suffices in making the diagnosis, although cross-sectional imaging (CT or MRI) is often used to assess the presence and extent of articular surface injury (reverse Hill-Sachs lesion), glenoid injury (reverse Bankart lesion) or ligamentous injury.
Plain radiograph
Posterior dislocation may be missed initially on frontal radiographs in 50% of cases, as the humeral head appears to be almost normally aligned with the glenoid . An axillary view is a preferred view for diagnosis. A Velpeau, Wallace or modified trauma axial view is an alternative . A scapular Y view has been shown to be unreliable for diagnosing posterior shoulder dislocations .
Radiographic findings include:
- absence of external rotation on images in a standard shoulder series is a clue
- lightbulb sign: fixed internal rotation of the humeral head which takes on a rounded appearance
- trough line sign: dense vertical line in the medial humeral head due to impaction of the humeral head
- loss of normal half-moon overlap sign, in which the glenoid fossa appears vacant due to the lateral displacement of the humeral head
- rim sign: widened glenohumeral joint >6 mm
- acute angle of the scapulohumeral arch (Moloney's arch) is also present and can be used to distinguish from anterior dislocation
Some associated injuries are recognized, including :
- reverse Hill-Sachs lesion
- reverse Bankart lesion
- proximal humeral fractures
- in particular fracture of the anatomical neck and/or lesser tuberosity
- posterior HAGL lesion
- posterior labrocapsular periosteal sleeve avulsion (POLPSA lesions)
Reporting checklist
In addition to stating that a posterior dislocation is present, any evidence of proximal humeral fractures or glenoid fractures should be sought and commented.
Treatment and prognosis
In most cases, acute posterior dislocations have spontaneously reduced prior to imaging .
When a posterior dislocation presents to the emergency department, unlike anterior shoulder dislocations which are relatively easily reduced, posterior dislocations are more problematic and attempts at closed reduction should only be performed in consultation with a treating orthopedic surgeon . Additionally, if the shoulder has been dislocated for 3 or more weeks (particularly common in debilitated elderly patients) or if the anterior humeral articular injury (reverse Hill-Sachs lesion) involves more than 20% of the articular surface, then the closed reduction is contraindicated .
Fortunately, neurovascular compromise is uncommon, but associated glenolabral and capsular injuries can lead to posterior shoulder instability .
Differential diagnosis
- shoulder pseudodislocation: on AP projection an inferiorly subluxed humeral head can mimic a posterior shoulder dislocation
See also
Siehe auch:
- Glühbirnenzeichen hintere Schulterluxation
- Schulterluxation
- lightbulb sign
- proximale Humerusfrakturen
- Hill-Sachs-Läsion
- vordere Schulterluxation
- Luxationen der oberen Extremität
- humeral avulsion of the glenohumeral ligament
- POLPSA lesion
- luxatio erecta
- glenohumerale Instabilität
- reverse Hill-Sachs and reverse Bankart lesions
- Trough-Linie
- inverse Hill-Sachs-Läsion (McLaughlin-Läsion)
- half moon overlap sign
- loss of normal half-moon overlap sign
- posterior shoulder subluxation
und weiter:

 Assoziationen und Differentialdiagnosen zu hintere Schulterluxation:
Assoziationen und Differentialdiagnosen zu hintere Schulterluxation:






