Rapunzel-Syndrom















Rapunzel syndrome is the term for a trichobezoar (gastric 'hair ball') which has a tail-like extension into the small bowel through the pylorus causing gastric outlet obstruction.
For discussion of other gastrointestinal foreign bodies, please see: bezoars.
Epidemiology
Trichobezoars are much more common in females (90%) than males. Of these cases in females, 80% of them primarily occur in children and adolescent females aged less than 30 years .
Risk factors
Risk factors include :
- trichotillomania
- trichophagia
- depression
- anxiety
- body dysmorphia
- prior surgeries
Clinical presentation
The symptoms of Rapunzel syndrome are caused either by gastric outlet obstruction or its complications and include:
- anorexia, bloating, early satiety
- weight loss
- vomiting immediately following meals
- acute epigastric pain
- patchy hair loss on the scalp
Complications
- obstructive jaundice
- mechanical small bowel obstruction
- small bowel mucosal erosion and ulceration
- small bowel perforation
- peritonitis
- acute pancreatitis
Pathology
Human hair (especially long hair) is resistant to digestion as well as peristalsis, so it tends to stay in the stomach and over a period of time may form a large ‘hair ball’. A trichobezoar may extend up to the pylorus, duodenum, or even jejunum. A part may break off into the small bowel and cause obstruction.
Radiographic features
Plain radiograph
- distended stomach shadow with an intragastric mottled gas pattern, outlined by fundal gas, which may resemble a food-filled stomach
- free gas shadow under diaphragm may be seen on an erect radiograph if bowel perforation is present
Fluoroscopy: barium study
- may show an intraluminal filling defect with mottled gas pattern without attachment to bowel wall
- over time the interstices of trichobezoar are filled with barium, this barium may remain for a considerable period of time and can be seen in delayed radiographs when the barium has exited the stomach and duodenum
Ultrasound
- may be seen as an echogenic mass with intense acoustic shadow seen within stomach and pylorus region
- complex intraperitoneal free fluid if complicated by bowel perforation
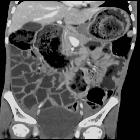
CT
- CT is the best imaging modality for showing the size and configuration of the trichobezoar and most accurately identifying its location
- may show an intragastric well-circumscribed inhomogenous mass consisting of ‘mottled gas pattern’ or ‘compressed concentric rings’ pattern due to the presence of entrapped air and food debris
- body of the mass in stomach while tail may extend to the duodenum or jejunum
- normal stomach wall can be traced completely separate from the lesion
- no contrast enhancement
- mucosal edema and wall thickening may be seen in duodenum and jejunum
- intraperitoneal fluid with free gas can be seen if perforation is present
Treatment and prognosis
Medical management is restricted to the correction of anemia and weakness. Pharmacological treatment in trichobezoars, unlike in some other types of bezoars, is normally ineffective .
The definitive treatment is essentially surgical. Laporotomy with the extraction of the bezoar is done with an exploration of the rest of the small bowel to look for detached bezoars. Small bowel segments showing extensive ulcerations and gangrene are resected.
Psychiatric evaluation is suggested for underlying illness.
Differential diagnosis
Although the imaging features allow confident diagnosis of trichobezoars, depending on the investigative modalities, the differentials to be considered are:
- gastrointestinal tumor such as a GIST extending into the stomach lumen
- other types of bezoar (e.g. phytobezoar)
Siehe auch:

 Assoziationen und Differentialdiagnosen zu Trichobezoar:
Assoziationen und Differentialdiagnosen zu Trichobezoar:

