retroperitoneal hemorrhage











Retroperitoneal hemorrhage can be a source of significant yet occult blood loss.
Terminology
Some articles conflate and/or confuse retroperitoneal hemorrhage and Wunderlich syndrome . However Wunderlich syndrome refers primarily to bleeding around the kidney, not the retroperitoneum in general, although of course retroperitoneal hemorrhage may occur secondary to Wunderlich syndrome.
Clinical presentation
The clinical features are varied depending on the amount of hemorrhage present, rate of onset and ability of the surrounding structures to contain the hemostatic system. The classic presenting features are:
- pain in the abdomen, flank or back
- shock
- palpable mass
- mass effect on the femoral nerve with resultant neuropathy has been described
However, presentation is often non-specific with a lack of cutaneous bruising or other localizing signs that can mean a delay in presentation and diagnosis.
Pathology
Etiology
- pelvic, abdominal or lumbar trauma (e.g. pelvic fractures)
- blood dyscrasia
- rupture arterial aneurysm (e.g. abdominal aortic aneurysm)
- interventional or surgical procedures
- bleeding from underlying renal or adrenal pathology (e.g. renal AML; renal trauma)
- rarely spontaneous retroperitoneal hemorrhage (SRH) - anticoagulation/fibrinolytic therapy
Radiographic features
The radiographic features can be variable depending on the stage of the hematoma.
Plain radiograph
Abdominal radiography is typically non-specific but may show:
- obliteration of psoas muscle outline
- displaced bowel loops
- in case of an aortic aneurysm as the cause, there may be calcification of aortic aneurysm giving a clue towards the cause in the correct correct clinical context
Ultrasound
- spillage of hemorrhage into the peritoneal cavity can be picked up
- a large hematoma in the retroperitoneum may be seen
- may show indirect evidence of displacement of retroperitoneal structures
- the presence of an abdominal aortic aneurysm with peri-aortic hemorrhage could favor a ruptured aortic aneurysm as the cause
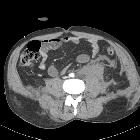
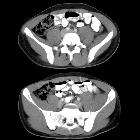
CT
- retroperitoneal structures have a hazy margin with fluid tracking through the retroperitoneum
- non-contrast
- acute and subacute hematomas - heterogeneous high attenuation
- chronic hematomas - low attenuation
- contrast-enhanced CT (without dedicated angiography)
- well-defined margin in case of a formed hematoma and absence of contrast enhancement
CT angiography
On angiography an active bleeding point or the breach in the wall of aneurysm (if its an underlying cause) may be identified.
MRI/MRA
On MRI a retroperitoneal hematoma has a variable appearance depending on the stage of the blood. It helps in better assessment as it can distinguish between blood and a neoplasm:
- acute and subacute stages: hyperintense on T1- and T2-weighted images
- chronic stage: hypointense is present on T1- and T2-weighted images
Treatment and prognosis
Management is based on the overall clinical context and vitals signs of the patient, the cause and stage of the hemorrhage.
Treatment
Medical
Initial medical management involves:
- correction of coagulation disorders
- reversal of any anticlotting therapies (e.g. octaplex for warfarin)
- intravenous fluid resuscitation
- blood transfusion
- admission to an appropriate level of care (e.g. HDU for significant bleeds)
Although no consensus guidelines exist for retroperitoneal hemorrhage, it is accepted that patients with small hematomas or without ongoing bleeding can be managed conservatively.
Interventional radiology
It was previously thought that spontaneous retroperitoneal hemorrhage is related to microvascular causes which cannot be treated endovascularly. However, endovascular treatments now have a proven role in management, including:
- stent graft placement
- arterial embolization
Chronic hematomas can become infected and are evacuated by percutaneous drainage or surgery. It has a better prognosis compared to that of the acute type.
Surgery
Inappropriate surgical evacuation can exacerbate hemorrhage by relieving hematoma induced tamponade. However, active retroperitoneal hemorrhage giving a large intra-abdominal hemoperitoneum can be fatal and can require emergency surgery.
Differential diagnosis
- psoas hematoma: often thought as a type of retroperitoneal hemorrhage but occurs posterior to the retroperitoneum in the iliopsoas compartment
Siehe auch:
- Wunderlich-Syndrom
- Nierenblutung
- retroperitonealer Abszess
- spontane retroperitoneale Einblutung
- intraabdominelle Blutungen
- eingeblutetes Angiomyolipom
- retroperitoneale Fibrose allgemein
- Hämatom im Musculus psoas
- traumatische Retroperitonealblutung
und weiter:

 Assoziationen und Differentialdiagnosen zu retroperitoneales Hämatom:
Assoziationen und Differentialdiagnosen zu retroperitoneales Hämatom:





