Inflammatory myofibroblastic tumor
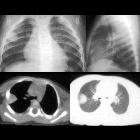
Infant with
respiratory distress. CXR AP shows a round opacity laterally in the right lung (above left) which projects in the middle of the chest over the trachea on the lateral (above right). Axial CT without contrast of the chest (below) shows the opacity to be a solid mass without calcification next to the pleura.The diagnosis was inflammatory myofibroblastic tumor.

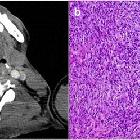
Inflammatory
myofibroblastic tumours: a pictorial review. PATHOLOGY: pararectal IMT. Axial and coronal reformations of contrast-enhanced CT on portal (a, b) and 8 min after injection delayed acquisitions (c, d). Pararectal solid and well-defined mass with moderated peripheral enhancement adjacent to the rectum and left seminal vesicle was detected. e Macroscopic view of the tumour after surgical resection. f Histological sample obtained after biopsy. Mesenchymal neoplasm composed of polygonal cells with clear cytoplasm and round normochromatic nuclei with abundant vessels and occasional scattered inflammatory cells was observed. Mixed within the neoplasm cells, there was a chronic inflammatory infiltrate of lymphoid cells. There were no foci of necrosis or mitotic figures

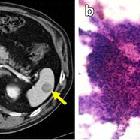
Imaging
findings of gastrointestinal tract tumors in children and adolescents. a, b A 3-year-old girl with inflammatory pseudotumor. She had fever and weight loss for the last 3–4 months. In physical examination, a mass was detected in the abdomen. a Axial fat-saturated T2-weighted image shows hypointense tumor in the ileum (arrows). b Post-contrast T1-weighted axial image shows peripherally contrast-enhanced tumor with central necrotic parts (arrows). After biopsy, ALK and SMA positive inflammatory pseudotumor was diagnosed

School ager
with a fever of unknown origin. Axial (left) and coronal (right) CT with contrast of the abdomen show a large, solid, heterogeneously enhancing mass in the left upper quadrant inferior to the stomach and spleen and anterior to the kidney whose organ of origin is uncertain.The diagnosis was inflammatory myofibroblastic tumor.

Inflammatory
myofibroblastic tumours: a pictorial review. PATHOLOGY: IMT of the iliopsoas muscle. a Axial and b coronal reformations of contrast-enhanced CT where an ill-defined and heterogeneous mass encompassing iliopsoas muscle and external iliac vessels, mimicking malignant sarcomatous neoplasm was observed. c Sample of the lesion obtained after surgical excision of the mass. Proliferation of fibroblast with a diffuse infiltration of lymphocytes, eosinophils and macrophages were found. No mitotic figures or cellular atypia were present. The mass was well-defined and no signs of invasiveness were found
Inflammatory
myofibroblastic tumours: a pictorial review. PATHOLOGY: IMT in the left supraglottic space (arrow) with paraglottic space involvement indicated by replacement of the paraglottic fat with soft tissue. a Axial reformation of contrast-enhanced neck CT. A solid, well-defined, little-enhancing nodule in the supraglottic larynx was observed (yellow arrow). It did not seem to infiltrate adjacent structures. b Microscopic study obtained after surgical removal of the lesion. The sample showed proliferation of fusiform cells mixed with macrophages and giant multinucleated cells. Small number of atypia and mitotic figures were present. The tumour presented an expansive growth pattern. Normal tissue was present in the peripheral zone (*)
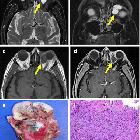
Inflammatory
myofibroblastic tumours: a pictorial review. PATHOLOGY: IMT of the left orbit. a, b Axial and coronal MR reformations of the same patient on T2-weighted sequences showed a well-delimited, hyperintense intraorbital mass, in the intraconal compartment, in the medial aspect. c, d T1-weighted images demonstrated a hypointense, homogeneous, well-delimited mass with peripheral enhancement after gadolinium injection. e Surgical sample obtained after resection. f Microscopic sample obtained after surgery demonstrated an epithelial tumour composed of fusiform cells mixed with an extensive chronic inflammatory infiltrate of plasmatic cells, lymphocytes and macrophages. In the peripheral of the sample striated muscle cells were also observed
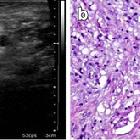
Inflammatory
myofibroblastic tumours: a pictorial review. PATHOLOGY: IMT of the epididymus. A 40-year-old man with a lump in the scrotum. a A hypoechoic, well-delimited epididymal lesion in the right scrotum was detected. b Sample of the epididymal lesion obtained after surgical resection of the mass. A diffuse infiltrate composed of fibroblastic and fusiform cells mixed with inflammatory cells (mainly lymphocytes and macrophages) was observed

Inflammatory
myofibroblastic tumours: a pictorial review. PATHOLOGY: paratesticular IMT. A 34-year-old man with no relevant medical history came to our hospital with a lump in the scrotum. a US showed an isoechoic, solid, paratesticular nodule with fine calcifications (yellow arrow). It did not seem to infiltrate the adjacent testicle. b Axial reformation of contrast-enhanced CT on portal phase demonstrated a well-delimited, heterogeneous, little-enhancing mass in the right scrotum. c Surgical sample obtained after orchiectomy. d Microscopic study of the lesion demonstrated a well-delimited lesion constituted of fibroblasts, lymphocytes and plasmatic cells with associated lymphoid follicle. There was no evidence of adjacent testicle invasion

Inflammatory
myofibroblastic tumours: a pictorial review. PATHOLOGY: IMT of the penis. A 46-year-old man with a mass in the penis came to our hospital. He related more than 6 years of slow growth of the mass with no suspicious associated symptoms. a, b Axial and coronal reformations of non-enhanced CT. Solid, well-defined, heterogeneous penile mass is shown. c, d Axial and coronal reformations of enhanced-CT after the injection of intravenous contrast on portal phase. The penile mass presents an heterogeneous and peripheral enhancement. e Surgical sample obtained after partial penectomy. Macroscopic view showed an heterogeneous aspect due to the mixture of tissues (solid tumour, lipoid component and areas of haemorrhage). f Microscopic study confirmed a mesenchymal tumour composed of fusiform cells, some of them multinucleated, with round or elongate nucleus. Prominent infiltrate of plasmatic cells and focal areas of haemorrhage were also found. No mitotic figures were observed

Inflammatory
myofibroblastic tumours: a pictorial review. PATHOLOGY: IMT of the liver. Axial reformations of T1-weighted MR before and after intravenous gadolinium injection. Well-defined, hypointense lesion on T1-weighted images (a) which presented weak enhancement in the arterial phase (b) and wash-out on portal and equilibrium phases (c-, d) located in hepatic left lobe. Capsule was present. e Macroscopic view of partial hepatectomy obtained after surgical excision of the lesion. A solid, well-defined and yellowing appearance mass is showed. f The lesion demostrated an expansive chronic inflammatory infiltrate of plasmatic cells, lymphocytes and macrophages. The nearby hepatocytes (*) were normal

Inflammatory
myofibroblastic tumours: a pictorial review. PATHOLOGY: hepatic IMT. a Abdominal ultrasound where a slightly hypoechoic, solid, heterogeneous mass arising in the left hepatic lobe was observed. Axial T1-weighted unenhanced (b) and contrast-enhanced MR images (c, d) showed an ill-defined with heterogeneous enhancement mass located in lateral hepatic segments. e, f Histological sample obtained after percutaneous biopsy. Mesenchymal tumour composed of fusiform cells, lymphocytes and lipid-filled macrophages can be observed. Normal hepatocytes with large and small fatty droplet change are also present
Inflammatory
myofibroblastic tumours: a pictorial review. PATHOLOGY: IMT of the spleen. a Axial reformation of contrast-enhanced CT on portal phase. Solid and well-defined lesion, hypodense to the surrounding spleen parenchyma. b Sample obtained with fine-needle aspiration. Prominent cellularity composed of an irregular, weakly basophil set of mioepithelial-fusiform cells. Numerous inflammatory cells (plasmatic, lymphocytes and few neutrophils and eosinophils) with isolated macrophages were also found. No atypia or mitotic figures were present

Inflammatory
myofibroblastic tumours: a pictorial review. PATHOLOGY: IMT of the stomach. Axial reformation of contrast-enhanced CT on arterial (a), portal (b) and 3 min after injection delayed (c) acquisitions. A well-defined, heterogeneous nodule with moderate enhancement on portal phase arising from the gastric fundus was found (yellow arrows). Diffuse liver steatosis can also be observed. d Microscopic studies performed after surgical removal of the lesion demonstrated high amount of mesenchymal fusiform cells combined with vascular structures. Small focis of inflammatory infiltrates were present. The lesion showed well-defined contours and an expansive growth pattern

Inflammatory
myofibroblastic tumours: a pictorial review. PATHOLOGY: metastatic IMT of the appendix. A 63-year-old man with antecedents of left hemicolectomy due to colon cancer. a Axial reformation of contrast-enhanced CT on portal phase acquired seven years after partial colectomy. An appendicular, irregular, solid mass with slight enhancement was identified (yellow arrow). Due to its radiological features, the lesion was diagnosed of appendicular carcinoma. The patient did not perform surgery. b Axial reformation of contrast-enhanced CT on portal phase performed 8 months later showed a significant growth of the appendicular mass with extension and infiltration of the adjacent small bowel loops. c Distant lymphadenopathy and liver metastases were present

ALK-1-positive
inflammatory myofibroblastic tumor of the thyroid complicated by Hashimoto’s thyroiditis: report of a rare case and a literature review. Echographic examination revealed a hypoechoic mass of with clear boundary (The arrow)

Inflammatory
myofibroblastic tumours: a pictorial review. PATHOLOGY: IMT of the lung. A 55-year-old man with a cough and haemoptysis.a Axial reformation of non-contrast CT with mediastinum window. Two solid, ill-defined nodules in right lower lobe are observed (yellow arrows). Note the air brocogram observed in the biggest mass. b Axial reformations with lung window of the same patient where the lung nodules are shown (white arrows). c Partial lobectomy of the right lower lobe specimen. Note the presence of the nodules (*). d Microscopic study of the resected lung sample where fusiform cells with an associated inflammatory infiltrate of lymphocytes, plasmatic cells and histiocytes was found

Inflammatory
myofibroblastic tumor • Inflammatory myofibroblastic tumor of the mesentery - Ganzer Fall bei Radiopaedia

Inflammatory
myofibroblastic tumor • Inflammatory myofibroblastic tumor - Ganzer Fall bei Radiopaedia

Inflammatory
myofibroblastic tumor • Inflammatory myofibroblastic tumor - Ganzer Fall bei Radiopaedia

Bladder
inflammatory myofibroblastic tumor: report of four cases. BIMT figures: a, b Cross-sectional view of the CT scans of patients diagnosed with bladder MIT. c, d Cystoscopic images

Unusual cause
of urinary retention in a child: inflammatory pseudotumor of the urinary bladder. Sagittal T1W image (a), T2W coronal image (b), and T2W FS axial image through the pelvis show polypoidal lesion arising from the bladder base (arrow in a, b, and c). The lesion is hypo- to isointense on T1W and mildly hyperintense on T2W with no suppression on fat-suppressed images. Patchy areas of diffusion restriction are seen (arrow in d)

Unusual cause
of urinary retention in a child: inflammatory pseudotumor of the urinary bladder. Transverse grayscale ultrasound (a) and color Doppler (b) image through the pelvis show well-marginated hypoechoic mass lesion (arrow in a and b) arising from the bladder neck projecting into the bladder lumen. The lesion shows mild vascularity

Inflammatory
Myofibroblastic Tumour (IMT) of the lung. CT without contrast: axial view with the lung window

Inflammatory
Myofibroblastic Tumour (IMT) of the lung. This figure demonstrates the heterogeneous enhancement of the lesion
Inflammatory
Myofibroblastic Tumour (IMT) of the lung. CT with contrast: sagittal view

Inflammatory
Myofibroblastic Tumour (IMT) of the lung. CT without contrast: sagittal view with the mediastinal window

Inflammatory
Myofibroblastic Tumour (IMT) of the lung. Sagittal image generated using MPR and averaging from original CT data

Young adult
with fever and respiratory distress. CXR AP and lateral (above) shows a well circumscribed, non-calcified, solid, round lesion in the right mid lung. AP image from a vintage tomogram (below) better demonstrates the lesion in the lung parenchyma.The diagnosis was inflammatory myofibroblastic tumor.
Inflammatory myofibroblastic tumors (IMT), also known as plasma cell granulomas, are rare neoplasms that have a diverse spectrum of biological behavior.
Terminology
These tumors were previously referred to as inflammatory pseudotumor.
Epidemiology
They can occur at any age and there is currently no recognized gender predilection.
Pathology
Composed of spindle cells (key feature) with a variable infiltrate of inflammatory cells and fibrous tissue. They can occur at numerous sites:
- more common
- lung: inflammatory myofibroblastic tumor of the lung
- abdominal cavity
- retroperitoneum
- extremities
- less common
- liver
- spleen
- genitourinary tract
Radiographic features
Imaging characteristics depend on the organ of involvement:
Siehe auch:
- inflammatorischer Pseudotumor der Orbita
- entzündlicher Pseudotumor der Lunge
- Inflammatorischer Pseudotumor der Harnblase
- inflammatorischer Pseudotumor der Leber
- inflammatorischer Pseudotumor der Milz
- inflammatorischer fibroider Polyp
- inflammatory pseudotumour IgG4 related disease
- inflammatorischer myofibroblastischer Tumor der Schilddrüse
und weiter:

 Assoziationen und Differentialdiagnosen zu inflammatorischer Pseudotumor:
Assoziationen und Differentialdiagnosen zu inflammatorischer Pseudotumor:inflammatorischer
myofibroblastischer Tumor der Schilddrüse





