cerebral cavernous malformation



















































Cerebral cavernous venous malformations, also commonly known as cavernous hemangiomas or cavernomas, are common cerebral vascular malformations, usually with characteristic appearances on MRI. It is the third most common cerebral vascular malformation after developmental venous anomaly and capillary telangeictasia.
Cavernous malformations are found throughout the body. This article focuses on cerebral cavernous venous malformations. For a general discussion and links to cavernomas in other locations, please refer to the general article on cavernous venous malformation.
Terminology
Many alternative terms have been used over the years including cavernous hemangioma, cerebral cavernous malformation or simply cavernoma. As these lesions are not neoplastic, it has been argued that the terms 'hemangioma' and 'cavernoma' should be avoided. Additionally, it is important to note that according to newer nomenclature (ISSVA classification of vascular anomalies) these lesions are now officially termed slow flow venous malformations.
Having said all that, it is probably helpful in reports to include the word 'cavernous' as this term is ubiquitous in the literature and most familiar to many clinicians.
For clarity and brevity, the term cavernous malformation is used for the remainder of this article.
Epidemiology
Most patients who present symptomatically do so at 40-60 years of age. Most patients have single lesions. Multiple lesions may be familial and screening of family members may be indicated (see familial multiple cavernous malformation syndrome). Additionally, cavernous malformations, along with capillary telangiectasias, are commonly seen following cerebral radiotherapy .
Clinical presentation
The majority of lesions remain asymptomatic throughout life and are found incidentally. Presentation due to hemorrhage may cause a headache, seizure or focal neurological deficit. The risk of hemorrhage is 1% per year for familial cases and somewhat less for sporadic lesions.
Pathology
Histologically cavernous malformations are composed of a "mulberry-like" cluster of hyalinized dilated thin-walled capillaries, with surrounding hemosiderin . These vessels are thrombosed to varying degrees. Unlike AVMs, there is no normal brain between the interstices of these lesions.
On occasion, they are intimately associated with a developmental venous anomaly (DVA), in which case they are known as a mixed vascular malformation.
Radiographic features
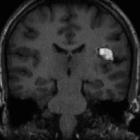
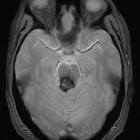
Cerebral cavernous malformations tend to be supratentorial (~80% cases) but can be found anywhere including the brainstem. They are usually solitary, although up to one-third of patients with sporadic lesions have more than one .
CT
Unless large, these lesions are difficult to see on CT. They do not enhance. If large they appear as a region of hyperdensity resembling blood products and speckles of calcification. If there has been a recent bleed then the lesion is more conspicuous and may be surrounded by a mantle of edema.
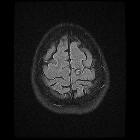
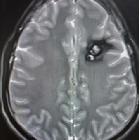
MRI
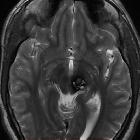
MRI is the modality of choice, demonstrating a characteristic “popcorn” or "berry" appearance with a rim of signal loss due to hemosiderin.
- T1: varied signal depending on the age of the blood products, small fluid-fluid levels may be evident
- T2
- hypointense rim
- varied signal internally depending on the age of blood products
- if a recent bleed has occurred, surrounding edema may be present
- GRE T2*/SWI
- prominent blooming
- useful for detecting smaller lesions otherwise missed by conventional spin echo sequences, especially in patients with familial or multiple cavernous malformations
- T1 C+ (Gd): generally no enhancement, although possible
Cavernous malformations can be grouped into four types based on MRI appearances using the Zabramski classification .
Angiography (DSA)
Cavernous malformations are angiographically occult and do not demonstrate arteriovenous shunting.
Treatment and prognosis
Many cavernous malformations are asymptomatic and can be treated conservatively. Symptoms can relate to mass effect, epileptic activity or repeated hemorrhage. Symptomatic lesions should, when possible, be resected and complete resection is curative .
Differential diagnosis
The differential, when cavernous malformations are numerous, is that of other causes of cerebral microhemorrhages, including :
- cerebral amyloid angiopathy: usually numerous small foci
- chronic hypertensive encephalopathy: more common in the basal ganglia
- diffuse axonal injury (DAI)
- cerebral vasculitis
- radiation-induced vasculopathy
- hemorrhagic metastases
- Parry-Romberg syndrome
Larger lesions can mimic:
- hemorrhagic cerebral metastases
- hemorrhagic primary brain tumors (e.g. ependymoma, glioblastoma)
Calcified lesions, such as old neurocysticercosis, or other infections (e.g. tuberculoma) should also be considered.
Siehe auch:
- Developmental Venous Anomaly
- Zerebrale Amyloidangiopathie
- Kavernom
- Altersbestimmung Blutung MRT
- Diffuses axonales Schädelhirntrauma
- zerebrale Mikroblutungen
- Zabramski Klassifikation zerebrale Kavernome
- progressive faziale Hemiatrophie
- eingeblutete Metastasen
- intraparenchymales Meningeom
und weiter:
- venöse Malformationen
- mixed vascular malformation
- spinale kavernomatöse Malformationen
- cavernous haemangiomas
- multiple cavernous haemangiomas of the brain
- cavernous malformation of the midbrain
- cavernous angioma mimicked by a loop of posterior inferior cerebellar artery
- zerebrale venöse Malformationen
- diffusion MRI of a cavernous angioma
- Developmental Venous Anomaly mit Verkalkungen

 Assoziationen und Differentialdiagnosen zu zerebrale Kavernome:
Assoziationen und Differentialdiagnosen zu zerebrale Kavernome:








