Dünndarmvolvulus















Midgut volvulus is a complication of malrotated bowel. It may result in proximal bowel obstruction with resultant ischemia if prompt treatment is not instigated.
Epidemiology
A midgut volvulus of malrotated bowel can potentially occur at any age but in approximately 75% of cases occur within a month of birth . Most of these are within the first week with 90% occuring within 1 year .
Clinical presentation
Typically the neonate is entirely normal for a period before suddenly presenting with bilious vomiting. If the volvulus does not spontaneously reduce, then the venous obstruction created by the superior mesenteric vein wrapped around the superior mesenteric artery results in venous obstruction and gradual onset of ischemia and eventual necrosis. As this occurs, the abdomen becomes swollen as fluid accumulates in the lumen of the bowel, and becomes tender. Eventually, peritonitis and shock become established.
Pathology
Midgut volvulus occurs as a complication of intestinal malrotation.
Associations
These include :
Radiographic features
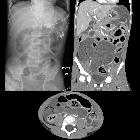
Plain radiograph
Unfortunately, plain radiographs are non-contributory appearing either normal early on or having appearances of bowel obstruction or even pneumoperitoneum later in the course of the disease.
Occasionally complete obstruction can lead to distension of the duodenal bulb and stomach leading to a double bubble sign .
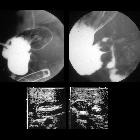
Fluoroscopy
A pediatric upper gastrointestinal contrast study is the examination of choice when the diagnosis is suspected. Not only is it able to identify the volvulus, but even in instances where spontaneous reduction has occurred, the underlying malrotation will be evident.
In the setting of volvulus findings include:
- corkscrew sign
- tapering or beaking of the bowel in complete obstruction
- malrotated bowel configuration
Contrast enemas have also been used historically. The theory being that in malrotation the large bowel will also be malrotated. Unfortunately, in 20-30% of cases, the cecum is normally located. The converse is also true, with the position of the cecum in normal individuals being variable .
Ultrasound
Ultrasound findings include :
- clockwise whirlpool sign
- abnormal superior mesenteric vessels
- inverted SMA/SMV relationship
- solitary hyperdynamic pulsating SMA
- truncated SMA
- inapparent SMV
- abnormal bowel
- dilated duodenum proximal to the obstruction
- thickened wall of small bowel distal to the obstruction
- dilated fluid-filled loops of small bowel
- free intra-abdominal fluid
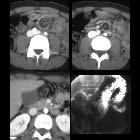
CT
CT is often carried out in older patients, in which presentation is non-specific.
Findings include:
- whirlpool sign of twisted mesentery
- malrotated bowel configuration
- inverted SMA/SMV relationship
- bowel obstruction
- free fluid/free gas in advanced cases
Treatment and prognosis
Urgent surgical repair (Ladd procedure) is required to prevent ischemia or to resect infarcted bowel loops. If resection is performed stomas are usually created. Additionally, the Ladd bands are divided and the mesenteric pedicle widened. In some instances, pexy (surgical fixation) of the duodenum and cecum may be performed although it is unclear if this is of benefit in preventing recurrence . It should be noted that normal anatomical positioning is not achieved; the duodenum and small bowel remain on the right, and the cecum and colon are on the left side of the abdomen .
Prognosis is dependent on the state of the small bowel and presence of systemic shock. In cases where no ischemia of the bowel is present, and the child is otherwise well, the prognosis is extremely good. Overall mortality of 3-9% is reported .
Small bowel obstruction for adhesions is seen a distant complication in 5-10% of cases.
Differential diagnosis
Vomiting in infancy has numerous causes and needs to be distinguished from normal possetting. Differential of a proximal obstruction includes :
- pyloric stenosis: vomiting will be non-bilious and projectile
- congenital obstruction
- meconium ileus
- intussusception
- external compression of the dudenum
- choledochal cyst
- mesenteric duplication cyst
- intramural duodenal hematoma
- preduodenal portal vein
- retroperitoneal tumor
- superior mesenteric artery syndrome
Siehe auch:
- innere Hernien
- Arteria-mesenterica-superior-Syndrom
- Mekoniumileus
- Volvulus
- Gastroschisis
- Choledochuszyste
- Pancreas anulare
- Invagination
- hypertrophe Pylorusstenose
- Bridenileus
- Duodenalatresie
- duodenales Web
- Duodenalhämatom
- intestinale Malrotation mit Volvulus
- intestinal atresia
und weiter:
- Dünndarmileus
- Whirlpool-Zeichen
- Double-Bubble-Zeichen
- corkscrew sign
- football sign
- intestinale Malrotation ohne Volvulus
- neonatal bilious vomiting
- internal hernia complicated by small bowel volvulus
- Malrotation mit Dünndarm-Volvulus
- small bowel volvulus due to midgut malrotation
- Dünndarmvolvulus durch Meckel-Divertikel

 Assoziationen und Differentialdiagnosen zu Dünndarmvolvulus:
Assoziationen und Differentialdiagnosen zu Dünndarmvolvulus: