infantile myofibromatosis
Myofibromas are benign neoplasms of soft tissues of myofibroblastic differentiation.
Terminology
'Myofibroma' is used for solitary lesions and 'myofibromatosis' for multicentric lesions.
Epidemiology
Myofibromas can occur at any age, but most predominantly occur in infants and young children, especially before the age of 2 years .
Clinical presentation
Can be asymptomatic. If present, symptoms and signs are nonspecific . Cutaneous myofibromas may present as purplish macules, resembling a vascular neoplasm.
Pathology
Myofibromas can be considered part of a large group of mesenchymal neoplasms called "fibroblastic and myofibroblastic tumors" or "musculoskeletal fibromatoses" that include a broad spectrum of benign, intermediate, and malignant tumors with overlapping histopathology.
In 2002, the WHO classified myofibromas under "pericytic (perivascular) tumors" .
Location
In children, there is a predilection for the head and neck regions > trunk > lower extremities > upper extremities > the viscera. Involved organs include the lungs, heart, gastrointestinal tract, liver, kidney, pancreas, or central nervous system.
In adults, myofibromas prefer the dermis, subcutis, or oral cavity >> deeper lesions in bone, muscle, or aponeurosis. Osseous lesions usually involve craniofacial bones.
Subtypes
There are three main subtypes of myofibromatosis :
- solitary
- multicentric without visceral involvement
- multicentric with visceral involvement
Genetics
Most cases are sporadic. However, reports of familial occurrence suggest a possible autosomal dominant or recessive inheritance in some cases of infantile myofibromatosis, which have been linked to mutations in the PDGFR-beta and NOTCH3 genes .
Radiographic features
Findings are usually nonspecific with a broad differential diagnosis .
Plain radiograph
- may not be visible
- possible dystrophic calcifications
- may be lytic if intraosseous
Ultrasound
- greyscale: solid hypoechoic mass, central hypo- to anechoic portion due to necrosis
- color Doppler: variable echogenicity
CT
- isodense to muscle
- osseous erosion, if adjacent to bone
- possible central necrosis
- possible dystrophic calcifications
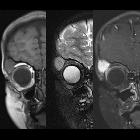
MRI
- ovoid and well-circumscribed
- may have a target sign due to central necrosis
Signal characteristics:
- T1: isointense to muscle
- T2: hyperintense
- T1 C+ (Gd): avid enhancement
Treatment and prognosis
Treatment includes observation or complete local excision. If resected, recurrence rate reported as 7-10% . Generalized myofibromatosis involving the viscera can be treated with chemotherapy .
History and etymology
Myofibromatosis was initially described by Williams and Schrum in 1951, when it was referred to as "congenital fibrosarcoma" . This entity was later renamed "congenital generalized fibromatosis" by Stout in 1954 , only to be again renamed "infantile fibromatosis" by Chung and Enzinger .
In its 2002 classification of soft tissue tumors, the WHO, recognized myofibromatosis under the benign category of fibroblastic-myofibroblastic lesions .
Differential diagnosis
Differential diagnosis depends on location. For differential diagnoses of a soft tissue location (such as intramuscular):
- nerve sheath tumor
- malignant peripheral nerve sheath tumor
- intramuscular myxoma
- synovial sarcoma
- hemangioma
- metastasis
Practical points
In practice, a well-circumscribed soft tissue lesion with avid enhancement has a very wide differential. For this reason, biopsy is required to make a definitive diagnosis . Given how uncommon myofibromas are compared to nerve sheath tumors and other diagnoses, myofibromas will often be very low on the differential.
See also
Siehe auch:
- Hämangiom
- Neurofibrom
- Lymphangiom
- Desmoid-Tumor - aggressive Fibromatose
- infantiles Fibrosarkom
- Leiomyofibrom
- Myoperizytom
- entzündlicher myofibroblastischer Tumor
- Langerhans-Zell-Histiozytose
und weiter:

 Assoziationen und Differentialdiagnosen zu Infantile Myofibromatose:
Assoziationen und Differentialdiagnosen zu Infantile Myofibromatose:




