schwannoma








































Schwannomas, less commonly called neurinomas or neurilemmomas, are benign tumors of Schwann cell origin and are the most common tumor of peripheral nerves, including cranial nerves.
This article provides a general overview of schwannomas. For a discussion of schwannomas located at specific sites, please refer to the relevant articles listed below.
Epidemiology
Peak presentation is in the 5-6 decades. When they occur in patients with neurofibromatosis type 2 (NF2), schwannomas usually present by the 3 decade . There is no sex predilection.
Associations
Most schwannomas are solitary (90%) and sporadic, however, there is an association with NF2 (abnormality of chromosome 22). Multiple schwannomas are characteristic of NF2. Approximately 18% of solitary schwannomas occur in patients with NF2 .
There is also schwannomatosis, which consists of multiple schwannomas without the concomitant involvement of cranial nerve VIII.
Clinical presentation
Presentation depends on the location of the tumor (see below) but generally, symptoms are due to local mass effect or dysfunction of the nerve they arise from.
Pathology
Macroscopic appearance
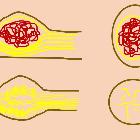
Schwannomas are benign encapsulated neoplasms of Schwann cells (WHO grade I). They arise eccentrically from their parent nerve, with the nerve fibers splayed along their surface (as distinct to neurofibromas which arise within the nerve).
Microscopic appearance
Conventional schwannomas are composed of spindle cells which demonstrate two growth patterns: Antoni type A and Antoni type B .
Antoni type A pattern: elongated cells are densely packed and arranged in fascicles. Palisades are sometimes seen; when prominent these form Verocay bodies.
Antoni type B pattern cells are less compact and are prone to cystic degeneration.
Variants
Schwannoma variants include :
- ancient schwannoma
- cellular schwannoma
- predominantly composed of Antoni A tissue
- no Verocay bodies
- most commonly found in a paravertebral location, or trigeminal nerves (CN V)
- melanotic schwannoma: dense melanin pigment
- plexiform schwannoma
- usually arise from skin or subcutaneous tissues
- usually diagnosed at birth or childhood
- usually sporadic, but rarely associated with NF2
- should not be confused with plexiform neurofibromas
- associated with NF1
- may undergo malignant change
Locations
- intracranial schwannomas
- cranial nerves: although almost any cranial nerve may be involved, except olfactory nerves and optic nerves which lack sheaths composed of Schwann cells, by far the most commonly involved nerve is the vestibulocochlear nerve (CN VIII)
- non-cranial nerve or intracerebral (very rare)
- spinal schwannoma
- arising from spinal nerve roots
- trunk
- intercostal nerves – see intercostal nerve schwannoma
- posterior mediastinum
- retroperitoneum
- gastrointestinal schwannoma
- limbs
- especially flexor surfaces (specifically ulnar and peroneal nerves)
Radiographic features
General imaging features of schwannomas include:
- well-circumscribed masses which displace adjacent structures without direct invasion
- cystic and fatty degeneration is common
- the larger a schwannoma, the more likely it is to show heterogeneity because of cystic degeneration or hemorrhage
- hemorrhage occurs in 5% of cases
- calcification is rare
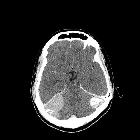
CT
CT is not as sensitive or specific for the diagnosis of schwannoma as MRI but is often the first investigation obtained. It is particularly useful in assessing bony changes adjacent to the tumor.
Imaging features include:
- low to intermediate attenuation
- intense contrast enhancement
- small tumors typically demonstrate homogeneous enhancement
- larger tumors may show heterogeneous enhancement
- adjacent bone remodeling with smooth corticated edges
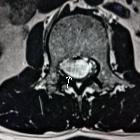
MRI
Schwannomas have fairly predictable signal characteristics :
- T1: isointense or hypointense
- T1 C+ (Gd): intense enhancement
- T2: heterogeneously hyperintense (Antoni A: relatively low, Antoni B: high)
- cystic degenerative areas may be present, especially in larger tumors
- T2*: larger tumors often have areas of hemosiderin
A number of signs can also be useful:
- split-fat sign: thin peripheral rim of fat best seen on planes along long axis of the lesion in non-fat-suppressed sequences
- target sign
- peripheral high T2 signal
- central low signal
- rarely seen intracranially
- fascicular sign: multiple small ring-like structures
Treatment and prognosis
Schwannomas are slow-growing lesions. Surgery is the treatment of choice. As schwannomas do not infiltrate the parent nerve, they can usually be separated from it. Recurrence is unusual, even after complete resection. They almost never undergo malignant change.
Siehe auch:
- Paragangliom
- spinale Schwannome
- spinal paraganglioma
- Neurofibrom
- neoplasms of the spinal canal
- Vestibularisschwannom
- spinal neurofibroma
- intradural extramedullary metastases
- intraspinales Meningeom
- benigner peripherer Nervenscheidentumor
- spinale Metastasen
- spinales Ependymom des Filum terminale
- Schwannom der Cauda equina
- Neoplasien der Cauda equina
- schwannomatosis
- paraspinal mass
- spinal nerve sheath tumours
- intradurale extramedulläre Tumoren
- Schwannome der Cauda equina bei Neurofibromatose Typ 2
- Schwannom der BWS
- Unterscheidung Schwannom Neurofibrom
- schwannoma of the cervical spine
- Spinal nerve roots
- Jugular foramen (CN IX, X, XI)
und weiter:
- Rippenusuren
- Läsionen der Felsenbeinspitze
- Cholesteatom
- laterale Halszyste
- vertebrale Metastasen
- carotid space
- Tumor Kleinhirnbrückenwinkel
- WHO-Klassifikation der Tumoren des zentralen Nervensystems
- neuroradiologisches Curriculum
- maligner peripherer Nervenscheidentumor (MPNST)
- erworbenes Cholesteatom
- Tumoren des hinteren Mediastinums
- Cholesteatom des äußeren Gehörgangs
- neurinoma of the trigeminal nerve
- posterior mediastinal masses
- Tumoren der Thoraxwand
- oberflächliche Weichteilläsionen der Extremitäten
- Neurofibromatose Typ 2
- Vernet syndrome
- neurofibromatosis type 2 (mnemonic)
- Zyste oder Fistel des zweiten Kiemenbogens
- paraspinal ganglioneuroma
- jugular foramen schwannoma
- Weichteiltumoren der Extremitäten
- posterior mediastinal mass in the exam
- Spasmus hemifacialis
- Raumforderungen im oder am Sinus cavernosus
- Schwannome des Gastrointestinaltraktes
- Zyste oder Fistel des vierten Kiemenbogens
- Schwannom Nervus vagus
- intralabyrinthine schwannoma
- schwannoma of the hypoglossal nerve
- Schwannom Nervus ulnaris
- neurogenic tumours
- Läsionen der Mandibula
- neuroma
- schwannoma nervus accesorius
- Nervenscheidentumor
- Schwannom des Nervus medianus
- Schwannom des Nervus facialis
- Schwannom Nervus ischiadicus
- Schwannom Nervus radialis
- neurilemmoma
- neurilemmomatosis
- Dumbbell schwannoma
- Schwannom der LWS
- Schwannom Fuß
- Schwannom des Nervus intercostalis
- schwannoma of the brachial plexus
- geniculate ganglia schwannoma
- schwannoma of the wrist
- Schwannom in der Fossa infratemporalis
- retroperitoneales Schwannom
- schwannoma causing posterior interosseous nerve impingement
- mediastinal schwannoma
- lumbales zystisches Schwannom
- Schwannom PET
- cervical schwannoma
- intrapelvic schwannoma
- tibial nerve schwannoma
- Faszikel-Zeichen
- intraosseous schwannoma
- schwannoma of the peroneal nerve
- präsakrales Schwannom

 Assoziationen und Differentialdiagnosen zu Schwannom:
Assoziationen und Differentialdiagnosen zu Schwannom: