intracranial schwannoma













Intracranial schwannomas (also referred to as neurinomas) are common benign tumors, accounting for 6-8% of all intracranial tumors, with the vast majority arising from the vestibular division of the vestibulocochlear cranial nerve .
Schwannomas can occur essentially anywhere in the body – see the general schwannoma article.
Epidemiology
Schwannomas are most frequently encountered in middle-aged and elderly adults with a predilection for females (F:M = 1.5-2:1), although they are found in all age groups.
Clinical presentation
Clinical presentation depends on both the size of the tumor, the nerve of origin and the exact location. In general, they will present with symptoms pertaining to the parent cranial nerve. Larger tumors will also exert mass effect on adjacent structures. Specific clinical features are discussed separately according to location:
Multiple schwannomas are a characteristic of neurofibromatosis type 2 (NF2). In this setting, any cranial nerve can be involved, including those that are very rarely seen in sporadic cases (e.g. oculomotor nerve) .
Pathology
Please refer to the generic article on schwannomas for a discussion of pathology.
Location
Almost all intracranial schwannomas arise from cranial nerves. Although any cranial nerve may be involved (except olfactory nerves and optic nerves which lack sheaths composed of Schwann cells) the rate of involvement is very skewed towards a few nerves primarily sensory nerves. Pure motor nerves rarely involved. The commonly involved cranial nerves are :
- vestibulocochlear nerve (CN VIII): see vestibular neuroma
- by far the most commonly involved nerve (90%)
- usually the superior portion of the vestibular division
- the cochlear division is almost never involved
- trigeminal nerve (CN V): see trigeminal schwannoma
- 2 most common
- facial nerve (CN VII): see facial nerve schwannoma
- 3most common
- cranial nerves of the jugular foramen (CN IX, X, XI): see jugular foramen schwannoma
In contrast, the other cranial nerves are rarely involved, most commonly seen in a patient with NF2 . Rarer still is non-cranial nerve or intracerebral (very rare) schwannomas .
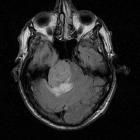
Radiographic features
Although the appearance of individual schwannomas will be influenced by the nerve of origin, composition (Antoni type B typically demonstrate higher T2 signal) and surrounding anatomy, they naturally share similar imaging characteristics.
Of note, the target sign which can be seen in neurogenic tumors elsewhere in the body (usually neurofibromas, but also sometimes in schwannomas) is essentially never encountered intracranially .
CT
Schwannomas are typically isodense to the brain and can be difficult to identify, depending on location. Cystic areas (usually found in larger tumors) are hypodense, similar to CSF. Following administration of contrast, they moderately enhance, often heterogeneously due to cystic areas .
Bone algorithm is excellent at assessing bony margins, especially useful when the tumor extends into or through a foramen. As these lesions are slow-growing they remodel the bone, with smooth borders, rather than destroy the bone .
MRI
MRI is the investigation of choice for assessment of intracranial schwannomas, not only due to greater contrast resolution but also exquisite anatomical details, which allows for precise localization of the tumor. This is particularly the case with high-resolution T2 sequences (e.g. FIESTA, CISS, SPACE).
Typical signal characteristics are :
- T1
- isointense to hypointense to brain
- low signal cystic areas, if present
- T1 C+ (Gd)
- prominent enhancement
- heterogeneous in 70% of cases
- T2
- typically somewhat hyperintense to brain
- cystic areas are hyperintense
- T2* (GE / SWI)
- hemosiderin staining may be encountered, particularly in larger tumors
- DWI/ADC
- often higher signal on both DWI and ADC (T2 shine through - not restricted diffusion)
Treatment and prognosis
Although the details of therapeutic options will depend on the location of the tumor, size and patient circumstances, generally surgical resection is curative if complete resection is achieved.
Radiotherapy is an alternative to surgery.
Differential diagnosis
The differential diagnosis will depend mostly on the specific location of the tumor and which nerve it arises from. As such, this is discussed separately in individual articles (see above).
Siehe auch:
- spinale Schwannome
- trigeminal schwannoma
- Vestibularisschwannom
- Neurofibromatose Typ 2
- jugular schwannoma
- Schwannom des Nervus facialis
- t2 shine through
- Schwannome der Hirnnerven
und weiter:

 Assoziationen und Differentialdiagnosen zu intrakraniale Schwannome:
Assoziationen und Differentialdiagnosen zu intrakraniale Schwannome:




