trigeminal schwannoma








Trigeminal schwannomas are uncommon slow-growing encapsulated tumors composed of schwann cells. They are the second most common intracranial schwannoma, far less common than vestibular schwannoma, and has a predominantly benign growth.
Epidemiology
Patients usually present in middle age, typically the 3to 4decades. They make up a third of tumors of Meckel's cave while accounting for less than 0.2% of all intracranial tumors. They are the most common intrinsic trigeminal neoplasm . Although intracranial schwannomas are common, making up approximately 8% of all intracranial tumors, the vast majority, around 90%, are vestibular schwannomas.
As with other schwannomas there is an association with neurofibromatosis type 2.
Clinical presentation
Typically, clinical presentation relates to trigeminal nerve dysfunction, e.g. neuralgia, neurasthenia or numbness. If large, then mass effect symptoms may be present. There may be a slight female predilection.
Radiographic features
Trigeminal schwannomas share the imaging findings of schwannomas elsewhere. They can have a dumbbell appearance when they extend both in the cisternal and Meckel cave, with a waist at the porus trigeminus . They can, however, if small, be confined to one compartment or section of the nerve :
- preganglionic (cisternal)
- confined to the prepontine cistern and cerebellopontine angle cistern
- second most common
- ganglionic (trigeminal ganglion)
- confined to Meckel cave
- most common
- postganglionic
- either confined to the cavernous sinus or extending through respective base of skull foramina, rarely confined to the extracranial compartment
- least common, accounting for 10% of cases
- most frequently involve the ophthalmic division, but can be found on all three divisions
CT
Schwannomas are typically isodense to brain, and can be difficult to identify, depending on location. Cystic areas (usually found in larger tumors) are hypodense, similar to CSF. Following administration of contrast they moderately enhance, often heterogeneously due to cystic areas.
Bone algorithm is excellent at assessing bony margins, especially useful when the tumor extends into or through a foramen. As these lesions are slow growing they remodel the bone, with smooth borders.
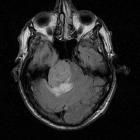
MRI
MRI is the investigation of choice for assessment of intracranial schwannomas, not only due to greater contrast resolution, but also exquisite anatomical details, which allows for precise localization of the tumor.
- T1
- typically isointense to brain
- cystic areas, if present, are hypointense
- T2
- typically somewhat hyperintense to brain
- cystic areas are hyperintense
- lesion in Meckel cave contrasts sharply on coronal T2 with contralateral normal, mostly CSF filled
- T1 C+
- prominent enhancement
- heterogenous in 70% of cases
- DWI/ADC
- often higher signal on both DWI and ADC (T2 shine through, not restricted diffusion)
Treatment and prognosis
Most lesions undergo surgical resection. They are in general benign lesions, and provided complete excision is feasible, then surgery is curative.
Differential diagnosis
The differential varies according to the size of the lesion and the location. In most cases, where the lesion is large and extends both into the cerebellopontine angle, the differential includes:
- vestibular schwannoma: ~80% of CPA masses
- meningioma: ~10% of CPA masses
- ependymoma
- metastasis
- chondrosarcoma
See: cerebellopontine angle mass for a more complete differential.
When small and confined to Meckel's cave the differential also includes:
- ICA aneurysms and vascular malformations
- pituitary macroadenoma
See: Meckel's cave mass for a more complete differential.
Siehe auch:
- Makroadenom Hypophyse
- Ependymom
- Schwannom
- Tumor Kleinhirnbrückenwinkel
- Vestibularisschwannom
- Metastase
- trigeminal nerve schwannoma in Meckel's cave
- Meckel's cave mass
- Schwannome der Hirnnerven
- zystisches Schwannom des Nervus trigeminus
und weiter:

 Assoziationen und Differentialdiagnosen zu trigeminal schwannoma:
Assoziationen und Differentialdiagnosen zu trigeminal schwannoma:





