Peutz Jeghers syndrome




















Peutz-Jeghers syndrome is one of the polyposis syndromes. It has an autosomal dominant inheritance and is characterized by:
- multiple hamartomatous polyps, most commonly involving the small intestine (predominantly the ileum), but also colon and stomach; mouth and esophagus are spared
- mucocutaneous melanin pigmentation involving the mouth, fingers and toes
Epidemiology
Peutz-Jeghers syndrome has been reported to be as common as 1 in 8300 live births.
Clinical presentation
Findings on clinical examination include mucocutaneous hyperpigmented macules of the nose, buccal mucosa, axilla, hands, feet and genitalia . A clinical diagnosis can be made following histopathological confirmation of typical Peutz-Jeghers syndrome morphology in 2 or more intestinal polyps or after any number of polyps or hyperpigmented macules (in a characteristic location) with a positive family history .
Pathology
Peutz-Jeghers polyps are non-neoplastic hamartomas due to the proliferation of all three layers of the mucosa, which have a characteristic feature of a smooth muscle core continuous with muscularis mucosa in a tree-like branching pattern. This distinguishes them from the hamartomatous polyps of Cronkhite-Canada syndrome, juvenile polyposis and Cowden disease.
Patients are at increased risk of:
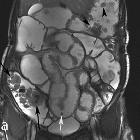
- intussusception
- GI tract adenocarcinoma, although the polyps themselves are not premalignant
- stomach: 29% lifetime risk
- small intestine: 13% lifetime risk
- extraintestinal malignancies
- adenoma malignum (adenocarcinoma subtype of the cervix)
- breast: 45-50% lifetime risk , more frequently ductal
- pancreas: 11-36% lifetime risk
- ovary: 18-21% lifetime risk , mainly sex cord tumors
- uterus: 9-10% lifetime risk
- cervix: 10-23% lifetime risk
- testis: 9% lifetime risk , large calcifying Sertoli cell tumors
- lung: 15-17% lifetime risk
Genetics
It is attributed to mutations in tumor suppressor genes, most commonly STK11 (70-94%) .
Treatment and prognosis
Due to the increased risk of malignancy, screening is generally recommended. Examples include annual mammography and contrast-enhanced breast MRI, beginning at 25 years of age; baseline CT/MR enterography at 8-10 years of age (and every 2-3 years from 18 years of age); MRCP or endoscopic US every 1-2 years beginning from 30-35 years of age .
History and etymology
The syndrome is named after Jans Peutz (1886-1957), a Dutch physician and Harold Jeghers (1904-1990), an American physician who had successively described the association between polyposis and the mucocutaneous macules.
Siehe auch:
- Invagination
- Cowden-Syndrom
- polyposis syndromes
- Adenoma malignum der Zervix uteri
- Kolonpolypen
- Peutz-Jeghers syndrome complicated by intussusception
- Dünndarmpolypen
- Polypen des Magens
- Cronkhite-Canada syndrome
- juvenile polyposis
und weiter:
- Kolorektales Karzinom
- Kolon
- ileokolische Invagination
- Polypen der Gallenblase
- Dünndarminvagination
- Dünndarmtumoren
- adenocarcinoma of the small bowel
- duodenal filling defects
- intestinale Invagination
- Koloninvagination
- complicated Peutz Jeghers syndrome
- Peutz Jeghers syndrome with small bowel obstruction
- Hamartom der Harnblase

 Assoziationen und Differentialdiagnosen zu Peutz-Jeghers-Syndrom:
Assoziationen und Differentialdiagnosen zu Peutz-Jeghers-Syndrom:



