subacute combined degeneration of the cord






















Subacute combined degeneration of the cord (SACD) is caused by vitamin B12 deficiency.
Epidemiology
Most common in patients older than 40 years and especially older than 60 years .
Clinical presentation
The clinical presentation of SACD is usually with loss of vibration and proprioception in the hands and feet, with eventual progression to sensory loss of all modalities, sensory gait ataxia, and distal muscle weakness, especially of the legs. Features of dementia may also become apparent.
Pathology
Etiology
SACD can be a sequelae of any cause of vitamin B12 deficiency. In the developed world where nutrition is generally adequate, it tends to result most commonly from pernicious anemia, but has other causes:
- Crohn disease and other causes of terminal ileitis (vitamin B12 is primarily absorbed at terminal ileum)
- use of proton pump inhibitors (acid is required to release vitamin B12 from meat)
- gastrointestinal surgery (especially if affecting the terminal ileum)
- celiac disease
- atrophic gastritis
- abuse of nitrous oxide (usually from recreational abuse)
Additionally, although uncommon, strict vegetarians or those who are undernourished may develop sufficient deficiencies to develop SACD.
Markers
Vitamin B12 levels may be normal in up to 30% of patients, and thus looking at levels of other more sensitive and specific biomarkers may be utilized instead:
- holotranscobalamin or active vitamin B12 (low)
- methylmalonic acid (high)
- homocysteine (high)
Radiographic features
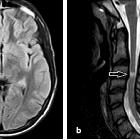
MRI
Most commonly there is symmetric bilateral high signal within the dorsal columns. This appearance has been described as the inverted "V" sign . The signal changes typically begin in the upper thoracic region, with ascending or descending progression .
The lateral corticospinal tracts, and sometimes lateral spinothalamic tract may also be involved. Although very unusual, there has been at least one described case of anterior cord involvement . Usually these areas have no contrast enhancement.
Often there is also accompanying cerebral white matter change. Both spinal and cerebral changes resolve after correction of vitamin B12 deficiency.
Treatment and prognosis
Management depends on the cause, but generally patients should be provided with intramuscular hydroxocobalamin injections, followed by oral supplementation. Additionally, patients should avoid using nitrous oxide.
Approximately half of all affected patients will completely recover .
Differential diagnosis
On imaging the differential includes:
- other nutritional or metabolic deficiencies/toxicities
- copper deficiency myeloneuropathy: may look identical
- vitamin E deficiency: may look identical
- methotrexate-induced myelopathy: appears identical
- demyelination
- multiple sclerosis: also affects dorsal columns but usually over a shorter length
- transverse myelitis: although longer length, usually not restricted to dorsal columns
- infectious causes
- HIV vacuolar myelopathy: may appear very similar
- herpes viruses myelitis
- neurosyphilis (tabes dorsalis)
- inflammatory processes
- ischemia
- neoplasms
- astrocytoma: not particularly of dorsal columns. usually, more cord expansion; often enhance
- ependymoma: not particularly of dorsal columns. usually, more cord expansion; often enhance
- hereditary syndromes
- leukoencephalopathy with brainstem and spinal cord involvement and lactate elevation: characteristically also involves the cerebral white matter and the brainstem
- Friedreich ataxia: also causes cervical cord atrophy ('thinning')
Siehe auch:
- Morbus Crohn
- Sarkoidose
- Ependymom
- Neurosarkoidose
- Transverse Myelitis
- Encephalomyelitis disseminata
- Astrozytom
- Demyelinisierende Erkrankung
- Neurolues
- spinales Ependymom
- spinales Astrozytom
- herpes viruses myelitis
- funikuläre Myelose MRT
- HIV vacuolar myelopathy
und weiter:

 Assoziationen und Differentialdiagnosen zu Funikuläre Myelose:
Assoziationen und Differentialdiagnosen zu Funikuläre Myelose: