superior cerebellar artery infarct




Superior cerebellar artery infarcts affect the superior cerebellar hemispheres, cerebellar vermis, and parts of the midbrain. The superior cerebellar artery is the most constantly identified vessel arising from the basilar artery with its origin just below the posterior cerebral artery in the distal segment.
Epidemiology
Cerebellar infarcts comprise ~2% of all acute brain infarcts. Up to half of these involve the region of the superior cerebellar artery .
Clinical presentation
Cerebellar infarction often presents with non-specific symptoms such as nausea/vomiting, headache, and dizziness making initial diagnosis challenging. Superior cerebellar artery infarction can present in two distinct patterns depending on the site of occlusion :
Pseudotumoral cerebellar infarction, which can be seen in posterior inferior cerebellar artery infarction, has not been described for superior cerebellar artery infarcts.
Pathology
Important causes of cerebellar infarction include atherosclerosis, cardiogenic emboli, and vertebral/basilar artery dissections . Proximal occlusions of the superior cerebellar arteries are often due to dissection or thrombosis, with peripheral occlusion typically due to embolization .
Radiographic features
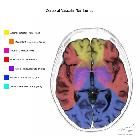
The imaging features are those of ischemic stroke in the vascular territory of the superior cerebellar artery: superior vermis, superior surface of the cerebellar hemispheres, much of the cerebellar white matter, and regions of the midbrain.
Siehe auch:

 Assoziationen und Differentialdiagnosen zu Infarkt im Versorgungsgebiet der Arteria cerebelli superior:
Assoziationen und Differentialdiagnosen zu Infarkt im Versorgungsgebiet der Arteria cerebelli superior:

