differential diagnosis for sacroiliitis






Sacroiliitis is an inflammation of one or both sacroiliac (SI) joints, and a common cause of buttocks or lower back pain. They can be a manifestation of a wide range of disease processes.
Clinical presentation
Symptoms of sacroiliitis can vary. People with sacroiliitis commonly present with ipsilateral or bilateral buttock and/or midline lower lumbar area pain. Up to 50% may have pain radiated to the lower extremity.
Pathology
The causes of sacroiliitis can be divided into unilateral or bilateral. See article: sacroiliitis (differential)
Radiographic features
Plain radiograph
Conventional radiography remains the first line of imaging despite its poor sensitivity and specificity in early disease. Specific sacroiliac joint views are helpful in the evaluation and comparing both sides of sacroiliac joints.
Radiograph findings include:
- sclerosis of the endplates particularly on the iliac side
- irregular joint end plates
- widening of joint spaces
CT
CT examinations offer greater sensitivity, accuracy and detailed information compared to plain radiography. However, due to higher radiation exposure, it is not advisable to use CT for diagnosis or follow-up purposes.
Nuclear medicine
Bone scans demonstrate increased radioisotope activity of the joints and helpful in localizing the source of the pain. It is also valuable in excluding stress fractures and other bone pathologies.
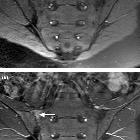
MRI
Though not routinely used for evaluating the sacroiliac joints, MRI is capable of identifying early inflammatory changes of joints when other imaging is negative and excludes other differential causes such a disc prolapse which may resemble clinical symptoms of sacroiliitis.
MRI features of sacroiliitis can be divided into inflammatory and structural lesions :
- marrow edema (first to appear): high signal on water sensitive sequences
- synovitis and capsulitis: thickening and contrast enhancement of the synovium and joint capsule
- enthesitis: thickening and contrast enhancement of ligaments and tendons at their attachments to bone
- subchondral sclerosis: bands of low signal (on all sequences) paralleling the joint margins, at least 5 mm from the joint space
- erosions: marginal foci of articular bone loss
- low T1 signal
- high T2/STIR signal if active
- more prominent anteroinferiorly and on the iliac side of the SIJ
- when confluent may appear as joint space widening
- periarticular fat deposition
- ankylosis
Classifications
- New York criteria (plain radiograph)
- ASAS sacroiliitis classification system (MRI)
Treatment and prognosis
Treatment would depend on the cause of the disease. Physiotherapy may also be helpful in strengthening the pelvic muscle and increase the mobilization of the SI joint. Analgesics such as NSAIDs may be useful in symptomatic management. Surgical fusion of the SI joint is considered the last resort when other conservative management is ineffective.
Differential diagnosis
The following conditions can mimic sacroiliitis:
- hyperparathyroidism: not true sacroiliitis but mimics its appearances
- osteitis condensans ilii: benign sclerosis on the iliac side of the joint
Siehe auch:
- Morbus Bechterew
- Morbus Crohn
- Rheumatoide Arthritis
- Gicht
- Osteitis condensans ilii
- Arthrose
- Colitis ulcerosa
- primärer Hyperparathyreoidismus
- Chronisch-entzündliche Darmerkrankungen
- Morbus Behçet
- Psoriasisarthritis
- Septische Arthritis
- SAPHO-Syndrom
- Rezidivierende Polychondritis
- Morbus Paget Os sacrum
- Iliosakralgelenksarthrose
- multi centric reticulohistiocytosis
- tuberkulöse Sakroiliitis
- Psoriasisarthritis ISG
- Sklerosierung Iliosakralgelenk bei Frauen
- New-York-Kriterien
- septic sacroiliitis
- sacroilitis grading
- Morbus Whipple
- grading of sacroiliitis
und weiter:

 Assoziationen und Differentialdiagnosen zu Sakroiliitis:
Assoziationen und Differentialdiagnosen zu Sakroiliitis: