Myositis ossificans















Myositis ossificans (MO) is the most common form of heterotopic ossification usually within large muscles. Its importance stems in large part from its ability to mimic more aggressive pathological processes. Myositis ossificans is one of the skeletal “don’t touch” lesions.
There are some conditions that are related to, or share a similar name to, myositis ossificans :
- myositis ossificans circumscripta: refers to new bone that usually appears after trauma
- myositis ossificans progressiva: a rare, inherited disorder characterized by fibrosing and ossification of muscle, tendon and ligaments of multiple sites that are disabling and ultimately fatal
- panniculitis ossificans: similar to MO but occurring in subcutaneous tissues
- fibro-osseous pseudotumor of the digits: variant of MO occurring in the fingers and toes
The remainder of this article focuses on the former. Myositis ossificans progressiva, panniculitis ossificans and fibro-osseous pseudotumor of the digits are discussed separately.
Epidemiology
Most cases of myositis ossificans occur as a result of trauma, and thus, the primary demographic is young adults . Another group which is especially prone to myositis ossificans are paraplegics, usually without evidence of trauma .
Clinical presentation
Typically presents as a painful, tender, enlarging mass, which in 80% of cases is located in large muscles of the extremities, often following recognized local trauma, although a definite traumatic event is not always recalled . In the case of paraplegics, recognized episodes of trauma are often absent, and the disease occurs particularly around the knees and hips .
Pathology
Myositis ossificans is essentially metaplasia of the intramuscular connective tissue resulting in extraosseous bone formation (without inflammation).
There are three well-described histopathological stages :
It has a zonal organization :
- peripheral, well-organized mature lamellar bone
- intermediate osteoid region
- central immature non-ossified cellular (fibroblasts) focus
Unfortunately, the histologically of myositis ossificans can appear similar to osteosarcoma, and thus, can lead to inappropriate management.
Radiographic features
The typical radiographic appearance of myositis ossificans is circumferential calcification with a lucent center and a radiolucent cleft (string sign) that separates the lesion from the cortex of the adjacent bone.
Plain radiograph
Initially calcification is absent but there may be soft tissue swelling. Calcification usually becomes apparent within 2-6 weeks, and the lesion reaches the classic well-circumscribed peripherally calcified appearance by two months. Over the following 4 or so months, they typically become smaller and denser .
The cleft between it and the subjacent bone may be difficult to see on plain radiographs.
CT
CT appearances are similar to those of plain radiography, demonstrating mineralization proceeding from the outer margins towards the center. The cleft between it and the subjacent bone is usually visible.
The peripheral rim of mineralization is usually visible within 4-6 weeks .
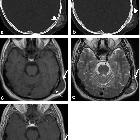
MRI
MRI appearances change with the age of the lesion.
Early features can be misleading because the peripheral calcification is not well seen, and edema in the soft tissues may extend beyond the often inapparent calcific rim.
- T1
- ill-defined isointense to muscle mass
- T2
- periphery: high signal (edema) seen up to 8 weeks
- central: heterogeneous high signal, due to high proliferating cellularity and cartilaginous components
- fluid-fluid levels have been reported and attributed to previous hemorrhage
- T1 C+ (Gd): enhancement is often present
Late features mimic bone :
- T1
- periphery: low signal (mature lamellar bone)
- central: intermediate to high signal (bone marrow)
- T2
- periphery: low signal (mature lamellar bone)
- central: intermediate to high signal (bone marrow)
- T1C+(Gd): usually none in mature lesions
Nuclear medicine
Non-specific increased bone scan uptake on flow and blood pool images is seen early on in the development of the lesion and gradually decreases as the lesion matures . Increased uptake on delayed phase is typical.
FDG PET can demonstrate intense uptake mimicking high-grade lesions .
Treatment and prognosis
Myositis ossificans is benign and there is no compelling evidence that malignant degeneration ever occurs . As such treatment is reserved for symptomatic lesions, and surgical resection is usually curative.
Differential diagnosis
Imaging differential considerations include:
- parosteal osteosarcoma: calcifies in the center and continues towards the periphery
- soft tissue sarcomas including
If fluid-fluid levels are present, then a different differential should be entertained (see differential of fluid-fluid level containing bone lesions).
See also
- soft-tissue calcification
- dystrophic soft-tissue calcification
- periarticular calcification
- calcific myonecrosis
Siehe auch:
- Osteosarkom
- Weichteilverkalkungen
- Pleomorphes Undifferenziertes Sarkom
- Synovialsarkom
- Heterotope Ossifikation
- Fibrodysplasia ossificans progressiva
- parossales Osteosarkom
- dystrophic soft-tissue calcification
- intramuskuläre Verkalkungen
- Myositis ossificans circumscripta
- fluid fluid level containing bone lesions
- Neuritis ossificans
und weiter:
- tumoröse Kalzinose
- Beckenfinger
- Melorheostose
- WHO Klassifikation der Weichteiltumoren
- skeletal mass with fluid-fluid levels
- Fasciitis nodularis
- Myositis
- differential diagnosis of intramuscular high STIR signal on MRI
- Muskelödem
- extraskelettales Chondrosarkom
- skelettale "do not touch"-Läsionen
- Flüssigkeit-Flüssigkeitsspiegel
- obturator nerve neuropathy
- string sign of parosteal osteosarcoma
- Merkspruch Weichteilverkalkungen
- breast myositis ossificans
- Myositis ossificans im Musculus psoas
- myositis ossificans of the gluteal muscles
- Myositis ossificans der Kaumuskulatur

 Assoziationen und Differentialdiagnosen zu Myositis ossificans:
Assoziationen und Differentialdiagnosen zu Myositis ossificans: