solitary bone plasmacytoma
Solitary bone plasmacytomas is an uncommon plasma cell tumor which is localized to bone. They may involve any bone, but they have a predisposition for the red marrow-containing axial skeleton:
- spinal disease is observed in ~50% (range 34-72%) of cases
- the thoracic vertebrae are most commonly involved, followed by lumbar, sacral, and cervical vertebrae
- the rib, sternum, clavicle, or scapula is involved in 20% of cases
Solitary bone plasmacytoma is one of the two subgroups of plasmacytoma, the other being the extramedullary plasmacytoma.
Epidemiology
- peak incidence is in 4to 6decades
- more common in males ~2:1
Clinical presentation
Physical findings are related to the site of involvement, presenting as a painful mass, pathologic fracture, or root or spinal cord compression syndrome.
The most common symptom of solitary bone plasmacytoma is a pain at the site of the skeletal lesion due to bone destruction by the infiltrating plasma cell tumor.
Patients with long bone involvement may present with pathologic fracture.
Diagnostic criteria
Diagnostic criteria for solitary bone plasmacytoma has been considered as follows :
- single area of destruction due to clonal plasma cells
- bone marrow plasma cell infiltration <5% of all nucleated cells
- absence of osteolytic bone lesions or other tissue involvement (i.e. no evidence of myeloma)
- absence of anemia, hypercalcemia or renal impairment (usually attributable to myeloma)
- low or absent serum/urine monoclonal protein
- preserved levels of uninvolved immunoglobulins
Radiographic features
Plain radiograph
Solitary expansile lytic lesion with thinning and destruction of the cortex, and bubbly/trabeculated appearance. Characteristically, the absence of sclerotic reaction is seen.
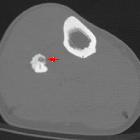
CT
Expansile lytic lesion with thinned out cortex and characteristic 'mini-brain' appearance has been described in solitary vertebral lesions.
MRI
A mini-brain appearance has also been described on MRI . It is seen as curvilinear low signal intensity areas within the lesion, giving an appearance of sulci in the brain. In fact, this appearance is so characteristic that it may obviate the need for a diagnostic biopsy.
Signal characteristics include:
- T1: hypo- to isointense
- T2: iso- to hyperintense to muscle
- T1 C+ (Gd): variable enhancement
Treatment and prognosis
Excision of the tumor and its extent is done, with chemo-radiotherapy as an adjuvant. Local recurrence is less than 5% and dissemination is seen in 35-70% of patients. The disease may progress to multiple myeloma, with a bad prognosis.
Differential diagnosis
General imaging differential considerations include:
- skeletal metastasis
- chronic osteomyelitis
- osteolytic metastasis
- osteoid osteoma
- osteoblastoma
- inclusion cyst
- Brown tumor of hyperparathyroidism
- aneurysmal bone cyst
- benign giant cell tumor
Siehe auch:
- Osteoid-Osteom
- Aneurysmatische Knochenzyste
- Multiples Myelom
- Osteolyse
- Riesenzelltumor
- Osteoblastom
- Knochenmetastasen
- Ostitis fibrosa cystica
- extraossäres Plasmozytom
- Knochenmarksinfiltration bei Plasmozytom
- smoldering myeloma
- Pariser Schema Plasmozytom
- Beckenosteolysen
- International Staging System (ISS) for myeloma
- Tübinger Schema Plasmozytom
- Monoklonale Gammopathie unklarer Signifikanz
- plasmacytoma of the skeletal system

 Assoziationen und Differentialdiagnosen zu Plasmozytom des Knochens solitär:
Assoziationen und Differentialdiagnosen zu Plasmozytom des Knochens solitär: