Osteoblastom




















Osteoblastomas are rare bone-forming tumors that may be locally aggressive. They are larger (>1.5-2 cm) and tend to affect the axial skeleton more often than their histologic relative, osteoid osteoma.
Epidemiology
They account for 1-3% of all primary bone tumors . Patients typically present around the second to third decades of life. There is a recognized male predilection with a male to female ratio of approximately 2.5:1.
Clinical presentation
With spinal lesions, painful scoliosis is a common presenting symptom. Otherwise, it presents with an insidious onset of dull pain, worse at night, with minimal response to salicylates (only 7% of patients respond, unlike osteoid osteoma). The area will characteristically be swollen and tender with a decreased range of motion.
Pathology
Osteoblastoma is histologically similar to an osteoid osteoma but they are larger. They are bone- and osteoid-forming and is comprised of osteoblasts. There is high associated vascularity.
Location
- spinal column: ~40% (range 32-46% ); often involves the posterior column
- cervical spine: 9-39% of all spinal lesions
- sacrum: 17% of all spinal lesions
- usually located in the metaphysis and distal diaphysis of the long bones
Variants
- aggressive (malignant) osteoblastoma: has a high of number epithelioid osteoblasts with nuclear atypia
Radiographic features
Osteoblastomas can have a wide range of radiographic patterns. Lesions are typically larger than 1.5-2 cm in size although smaller lesions may occur .
Plain radiograph
- lesions are predominantly lytic, with a rim of reactive sclerosis
- tend to be expansive
- internal calcification may sometimes be present
- an associated soft tissue mass may also be present
- demonstrate a rapid increase in size with associated cortical expansion in the vast majority of patients, sometimes with cortical destruction
- there may be surrounding sclerosis or periostitis in up to 50%
- there may be a secondary aneurysmal bone cyst in 20%
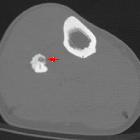
CT
- similar to the radiograph, lesions are often demonstrated as predominantly lytic
- internal matrix mineralization is better appreciated on CT
MRI
MRI features tend to be non-specific and often overestimate the lesion :
- T1: typically hypo to isointense on T1 with areas of decreased intensity that correspond to foci of calcification
- T2: typically isointense to hypointense on T2 with foci of decreased intensity corresponding to the foci of calcification
- a high signal may be seen in surrounding bone marrow and soft tissues due to edema "flare phenomenon"
- C+ (Gd): this is a highly vascular tumor and therefore typically avidly enhances, with associated enhancement of the surrounding soft tissues
Nuclear medicine
- Tc-99m MDP or HMDL: often shows intense uptake although this is non-specific and is typical in all lesions exhibiting increased bone turnover
Treatment and prognosis
Radical surgical excision is often the treatment of choice. Pre-operative embolization is commonly carried out to reduce bleeding risk although surgery needs to be performed at a very short time interval in order to avoid reconstitution of collateral blood supply. Percutaneous ablation is an emerging modality for treatment of these lesions (as well as osteoid osteoma) .
Complications
Lesions are prone to extensive intraoperative bleeding due to intrinsic vascularity.
Differential diagnosis
- osteoid osteoma: <1.5-2 cm
Siehe auch:
und weiter:
- vertebrale Metastasen
- Skoliose
- Osteom NNH
- Multiples Myelom
- kortikales Desmoid
- Tumoren der Nasennebenhöhlen
- solide Periostreaktion
- epiphysäre Knochentumoren
- radiologisches muskuloskelettales Curriculum
- Enchondroma protuberans
- osseous lesions preferentially involving the epiphysis
- solitary sclerotic bone lesion
- spinale Metastasen
- ivory vertebra sign
- ring- und bogenförmige Verkalkungen
- lytic bone lesion (mnemonic)
- Plasmozytom des Knochens solitär
- Läsionen des Sakrums
- Knochenläsionen der Epiphyse
- solitary sclerotic bone lesion with a lucent centre
- primary tumours of the spine
- bone-forming tumours
- Sklerosierung der Klavikula
- posterior vertebral body lesions (mnemonic)
- osteoid lesions
- lytic bone lesion surrounded by marked sclerosis (mnemonic)
- Knochenläsionen mit Sequester
- Osteoblastom der Halswirbelsäule
- spikulierte Periostreaktion
- Knochenläsionen der Metaphyse
- Osteoidosteom der Wirbelsäule
- vertebral osteoblastoma
- osteoblastoma sacrum
- osteoblastoma of the radius
- osteoblastoma of occipital bone
- osteoblastoma of hamate
- osteoblastoma of the skull
- knochenbildende Tumoren

 Assoziationen und Differentialdiagnosen zu Osteoblastom:
Assoziationen und Differentialdiagnosen zu Osteoblastom: