testicular teratoma
Testicular teratoma, unlike ovarian teratoma, is often aggressive in its biological behavior, and often exists as part of testicular mixed germ cell tumors.
Epidemiology
Pure testicular teratomas account for only 4-9% of all testicular tumors. A similar number are seen in the context of testicular mixed germ cell tumors (approximately 50% of these tumors contain teratomatous components, and they make up approximately 15% of all testicular germ cell tumors) .
The former is more commonly found in very young children (<2 years of age) whereas teratomas in the context of mixed germ cell tumors are more common in young adults (typically 20-30 years of age) .
Clinical presentation
The most common presentation of pure teratomas is with a painless testicular mass.
Pathology
Testicular teratomas are non-seminomatous germ-cell tumors and should be divided by age of the patient and by the degree of differentiation (into mature and immature).
Mature teratomas contain well-differentiated tissues and should be biologically indolent. In pre-pubertal cases, this is born out, whereas in post-pubertal males it is believed that mature teratomas represent fully differentiated teratocarcinomas with a precursor of embryonal carcinoma . As such, in post-pubertal males, even mature teratomas should be regarded as potentially aggressive. In fact, if the seminiferous tubules of the adjacent seemingly uninvolved testis are examined, cellular atypia and carcinoma in situ are often identified .
Immature teratomas are more common in the testes, although they are rare as pure tumors, usually associated with other non-seminomatous cell types (e.g. embryonal cell carcinoma, choriocarcinoma, yolk sac tumor) as part of a testicular mixed germ cell tumor .
In both cases, they contain cell populations derived from all three embryonal layers (ectoderm, mesoderm and endoderm) although the proportion of each need not be even remotely equal.
It is interesting to note that in addition to biological behavior, the chromosomal makeup of these tumors also depends on the age of the patients. Tumors in pre-pubertal patients are typically diploid, whereas in adults they tend to be hypotriploid .
Classification
See: classification of germ cell tumors.
Radiographic features
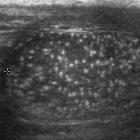
Ultrasound
This is the modality of choice for direct imaging of the testes with teratomas in the testes being similar in appearance to other locations. Mature teratomas tend to be cystic with heterogeneous echoes in the fluid representing a mixture of mucinous or sebaceous material with or without hair follicles. Solid components are present of variable echogenicity, including hyper-echoic and shadowing fatty components.
Immature teratomas tend to be more solid, but still heterogeneous on account of areas of hemorrhage and necrosis.
CT
CT is required to assess for nodal and distant metastatic disease.
The spread of testicular tumors is both lymphatic and haematogenous.
Testicular lymphatics ascends along the gonadal arteries such that right-sided tumors involve pericaval nodes (aortocaval nodes, precaval nodes, and right paracaval and retrocaval nodes) whereas left-sided tumors typically ascend to pre-aortic and left para-aortic nodes .
Haematogenous spread is typically to the lungs, as well as brain, bone and liver .
Staging
See: staging of testicular cancer
Treatment and prognosis
Treatment depends of the age of the patient, the stage and histology of the tumor.
In cases of entirely mature benign teratomas, orchiectomy may suffice, although in adults even apparently completely mature teratomas can have aggressive behavior, largely due to the potential of small components of embryonal carcinoma cells . In fact metastases of histologically mature tissues are sometimes seen (mature metastasizing teratoma).
Conversely in infants and young children, even though a tumor may contain foci of immature teratoma, mature teratomas have a benign clinical course . Overall age is thus the most important prognostic factor.
In cases of immature teratoma, treatment depends on the stage. For stage I tumors orchiectomy and surveillance may suffice. Alternatively, retroperitoneal nodal dissection and chemotherapy may be recommended .
In adults, approximately 30% of cases have metastases at the time of diagnosis .
Complications
Complications include:
- growing teratoma syndrome
- malignant degeneration of a mature teratoma:
- malignancy of any of the components, e.g. squamous cell carcinoma
- mature metastasizing teratoma
Differential diagnosis
- other testicular germ cell tumors
- testicular epidermoid cyst: overlap in appearance
- testicular metastases
- testicular lymphoma
- testicular infarction (e.g. secondary to testicular torsion)
- testicular abscess
Siehe auch:
und weiter:

 Assoziationen und Differentialdiagnosen zu Teratom des Hodens:
Assoziationen und Differentialdiagnosen zu Teratom des Hodens: