Diffuse alveolar hemorrhage (DAH)











Diffuse alveolar hemorrhage (DAH) is a subset of diffuse pulmonary hemorrhage when bleeding is diffuse and directly into the alveolar spaces. It can occur in a vast number of clinical situations and can be life-threatening.
Pathology
Blood tends to fill alveolar spaces at multiple sites.
Etiology
Causes include:
- pulmonary vasculitides (particularly small vessel vasculitides): a pulmonary capillaritis is considered the most common underlying lesion associated with diffuse alveolar hemorrhage
- ANCA associated pulmonary vasculitides
- non-ANCA associated pulmonary vasculitides: Goodpasture syndrome
- certain connective tissue disorders
- systemic lupus erythematosus : considered commonest associated connective tissue disorder to result in diffuse alveolar hemorrhage
- mixed connective tissue disease
- coagulative disorders
- medications: excessive antiplatelet therapy
- inhaled toxins
- conditions causing back pressure
- pulmonary hemorrhage complicating multifocal infection
- pulmonary hemorrhage complicating diffuse alveolar damage
- pulmonary hemorrhage complicating widespread pulmonary malignancy
- post bone marrow transplantation
- pulmonary hemosiderosis
- antiphospholipid syndrome
Radiographic features
Plain radiograph
The clinical context is crucial in image interpretation. The exact pattern may differ depending on the underlying cause. In general, the typical feature on plain film during an acute diffuse alveolar hemorrhage is a diffuse infiltrative opacification pattern . At times there may a slight predilection towards the mid zones with some apical sparing .
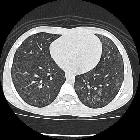
CT
The HRCT pattern can vary with time of onset of the hemorrhage and the clinical context is crucial in image interpretation:
- acute phase
- can range from lobular or lobar areas of ground-glass opacities to predominant consolidation
- ground-glass opacity is generated by subtotal alveolar filling with blood and is accompanied by the apparent prominence of segmental and subsegmental bronchi, which has been referred to as the “dark bronchus sign"
- 2–3 days
- intralobular lines and smooth interlobular septal thickening superimpose on areas of ground-glass opacity
- may sometimes give rise to a crazy-paving pattern
- these can often resolve
- between chronic recurrent bleeding events
- ill-defined centrilobular nodules
- reflecting an intra-alveolar accumulation of pulmonary macrophages
- usually uniform in size (1-3 mm)
- diffusely distributed
- no zonal predominance
- ill-defined centrilobular nodules
- with severe repeated hemorrhage: may progress with features of interstitial fibrosis
Complications
Repeated episodes can lead to organizing pneumonia, collagen deposition in small airways and ultimately pulmonary fibrosis .
See also
Siehe auch:
- Churg-Strauss-Syndrom
- Granulomatose mit Polyangiitis
- Lungenfibrose
- verdickte interlobuläre Septen
- systemischer Lupus Erythematodes
- Lungenblutung
- Alveolarproteinose
- Mitralklappeninsuffizienz
- Hämosiderose der Lunge
- Goodpasture-Syndrom
- crazy paving-Muster
- pulmonale Vaskulitis
- mixed connective tissue disease
- pulmonale venookklusive Erkrankung
- Mikroskopische Polyangiitis
- Mitralklappenstenose
- zentrilobuläre Lungennoduli
- idiopathic, pauci-immune pulmonary capillaritis (IPIPC)
- diffuse Lungenblutung
- diffuser Alveolarschaden
- ground-glass opacities
und weiter:

 Assoziationen und Differentialdiagnosen zu diffuse Alveolarblutung:
Assoziationen und Differentialdiagnosen zu diffuse Alveolarblutung: