pleural plaque




















Pleural plaques are the most common manifestation of asbestos-related disease and can be identified with a very high degree of specificity with CT.
Epidemiology
Pleural plaques are strongly associated with inhalational exposure to asbestos. There is an extremely long latency (typically 20 to 30 years) after the onset of exposure . As asbestos is primarily used in construction and machinery environments, asbestos-related diseases in general, including pleural plaques, are primarily seen in men.
Clinical presentation
Pleural plaques are asymptomatic and incidentally found on radiography of the chest.
Pathology
Fibers are thought to reach the pleural space via the lymphatic system. Macroscopically, pleural plaques appear as grey-white regions of pleural thickening, often thickest at the margins, giving rise to the holly leaf appearance (aside from the color of course).
Microscopically, they are composed of dense hyalinised collagen and are relatively acellular. The collagen is usually arranged in a loose 'basket-weave' pattern. Although asbestos fibers are sometimes seen, asbestos bodies are not a feature .
Radiographic features
Pleural plaques typically arise from the parietal pleura, most frequently from the lower portions of the chest, sparing the apices and costophrenic angles. They are also frequently found arising from the mediastinal pleura. Visceral pleura may also be involved infrequently. When such visceral plaques are present, they are typically associated with underlying parenchymal abnormalities and extensive pleural disease .
The plaques may be calcified; however, most (85-95%) are not .
Plain radiograph
Pleural plaques exhibit the so-called "incomplete border sign" on chest radiograph. The inner margin is often well-defined because it is tangential to the x-ray beam and the adjacent lung is a good contrast medium. The tapering outer margin is indistinct as it is en face to the x-ray beam and the chest wall provides less tissue contrast. Calcified plaques are more obvious than non-calcified plaques to be identified. Locations most commonly encountered include posterolateral, mediastinal, and diaphragmatic pleura . The appearance of plaques has been likened to that of a holly leaf, with thickened rolled and nodular edges .
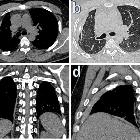
CT
CT is the modality of choice for assessment of pleural plaques as it is able to identify plaques anywhere in the chest, whether calcified or not. Sensitivity and specificity are both very high (95-100%) . With coronal and sagittal reconstructions, the diaphragmatic domes and apices are also well-imaged.
Visceral pleural plaques have a predilection for the interlobar fissures and are usually associated with adjacent parenchymal abnormalities. In some instances, short linear regions of fibrosis are seen extending radially away from the plaque (so-called hairy plaques) .
Treatment and prognosis
Pleural plaques are benign and require no treatment or follow-up. Occasionally, pleural plaques can migrate on interval scans .
Differential diagnosis
On plain film, consider:
- diffuse asbestos related pleural thickening: diffuse pleural thickening
- extrapleural fat
- rib fracture
- pleural tumors
- pleural pseudoplaques
On CT, consider:
- status post talc pleurodesis
- granulomatous disease such as pleural tuberculosis
See also
Siehe auch:
- Silikose
- Pleuraempyem
- Pleuramesotheliom
- Asbestose
- pleurale Tuberkulose
- Pleuraplaques bei Asbestose
- Talkosis
- Pleuritis
- Pleurodese
- localised mediastinal malignant mesothelioma
- asbestos related pleural disease
- Pleuritis exsudativa
- hyperdense Pleura
- hairy pleural plaques
- Pleuraverdickung
und weiter:

 Assoziationen und Differentialdiagnosen zu Pleuraplaques:
Assoziationen und Differentialdiagnosen zu Pleuraplaques: