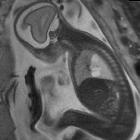
Polyhydramnion







Polyhydramnios refers to a situation where the amniotic fluid volume is more than expected for gestational age.
It is generally defined as:
- amniotic fluid index (AFI) >25 cm
- largest fluid pocket depth (maximal vertical pocket (MVP)) greater than 8 cm : although some centers, particularly in Australia, New Zealand, and the United Kingdom, use a cut off of 10 cm
- overall amniotic fluid volume larger than 1500-2000 cc
- two diameter pocket (TDP) >50 cm
Epidemiology
It can occur in approximately 1-1.5% of pregnancies.
Clinical presentation
The patient may clinically present as a large for dates uterus.
Pathology
Polyhydramnios occurs as a result of either increased production or decreased removal of amniotic fluid. The etiology of polyhydramnios can be due to a vast variety of maternal and fetal disorders.
It is usually detected after 20 weeks (often 3 trimester).
Causes
The potential causes of polyhydramnios are variable including:
- idiopathic: 60-65%: this is a diagnosis of exclusion despite accounting for a majority of cases, also termed idiopathic polyhydramnios
- maternal: 25-30%
- diabetes: commonly gestational diabetes
- maternal congestive heart failure
- fetal: 10-20%
- CNS lesions (e.g. neural tube defects): fetal CNS abnormalities tend to be the commonest out of all fetal causative associations
- proximal gastrointestinal obstruction
- gastrointestinal atresia(s)
- abdominal wall defects
- fetal intestinal volvulus, e.g. from an intestinal malrotation
- fetal cervicothoracic abnormalities
- fetal cervical masses
- thoracic masses
- fetal cardiovascular anomalies
- sustained fetal tachycardia (e.g. supraventricular tachycardia (SVT), atrial flutter, ventricular tachycardia)
- twin pregnancy-related complications
- twin-twin transfusion: occurs in the recipient
- hydrops fetalis: immune and non-immune
- fetal skeletal abnormalities
- reduced fetal movement
Associations
- fetal macrosomia: independent of maternal diabetes ,in the idiopathic form
- mesoblastic nephroma
- Pena Shokeir syndrome
- maternal overhydration
Polyhydramnios is associated with the poor outcome if present in combination with intrauterine growth restriction (IUGR); usually seen in aneuploidies 18,13, and 21.
Classification
This classification is general consensus based on common practices at the time of writing (July 2016) but this varies according to countries and gynecologist association guidelines.
Some classify the severity of polyhydramnios as
- mild: single deepest pocket at 8-11 cm or AFI 25-30
- moderate: single deepest pocket at 12-15 cm or AFI 30.1-35
- severe: single deepest pocket >16 cm or AFI >35
Complications
The risk of the following obstetric complications is increased when polyhydramnios is present due to over-expansion of the uterus:
- maternal dyspnea
- premature membrane rupture
- preterm labor
- abnormal fetal presentation
- umbilical cord prolapse
- postpartum hemorrhage: due to reduced uterine myometrial tone
Treatment and prognosis
The prognosis is variable dependent on associated conditions. Usually minimal or no interventional required for idiopathic mild uncomplicated cases. Options include:
- improved maternal diabetes control
- cesarian section if there is profound macrosomia
- therapeutic amniocentesis/amnioreduction
- Indomethacin
See also
Siehe auch:
- amniotic fluid index
- Gastroschisis
- Hydrops fetalis
- kongenitale pulmonale Atemwegsmalformation (CPAM)
- Ösophagusatresie
- Oligohydramnion
- Duodenalatresie
- Omphalozele
- Pena-Shokeir-Syndrom
- amniotic fluid volumes
- Neuralrohrdefekt
- kongenitale Zwerchfellhernie
- large for dates uterus
- kongenitales mesoblastisches Nephrom
- congenital high airways obstruction syndrome
- Makrosomie
- fetale Struma
- therapeutic amniocentesis
- kongenitales zervikales Teratom
- Teratom des Pharynx
- twin-twin transfusion
- CHAOS
- jejuno-ileal atresia
- maximal vertical pocket (MVP)
- two diameter pocket
- intra uterine growth restriction (IUGR)
- intestinal maltoration
und weiter:
- Pätau-Syndrom
- obstetric curriculum
- Beckwith-Wiedemann-Syndrom
- Mikrognathie
- Thanatophore Dysplasie
- fetal pleural effusion
- Lippen-Kiefer-Gaumen-Spalte
- Arthrogryposis multiplex congenita
- fetal conditions associated with maternal diabetes
- Ileumatresie
- caudal dysplasia sequence
- amniotic fluid volume
- Goldenhar-Gorlin-Syndrom
- sonographic values in obstetrics and gynaecology
- Mekoniumperitonitis
- Siamesische Zwillinge
- Pierre-Robin-Sequenz
- fetal akinesia / hypokinesia sequence
- fetal infection
- umbilical cord prolapse
- two diameter pocket method
- fetale Hirntumoren
- Bartter-Syndrom
- maximal vertical pocket method
- amnioreduction
- angeborene ösophagotracheale Fistel
- jejunoileal atresia
- feto-fetal transfusion syndrome
- antenatale Darmperforation

 Assoziationen und Differentialdiagnosen zu Polyhydramnion:
Assoziationen und Differentialdiagnosen zu Polyhydramnion: