Kiemenbogenzyste









Branchial cleft anomalies comprise of a spectrum of congenital defects that occur in the head and neck.
Pathology
The anomalies result from branchial apparatus (six arches; five clefts), which are the embryologic precursors of the earand the muscles, blood vessels, bones, cartilage, and mucosallining of the face, neck, and pharynx .
During the 3 to 5 week of embryonic development, the second arch grows caudally and covers the third, fourth and sixth arches. When it fuses to the skin caudal to these arches, the cervical sinus is formed. Eventually, the edges of cervical sinus fuse and the ectoderm within the tube disappears . Persistence of branchial cleft or pouch results in a cervical anomaly located along the anterior border of the sternocleidomastoid muscle from the tragus of the ear to the clavicle .
The range of anomalies can include:
- cyst: no internal or external communication
- fistula: communicates both internally and externally
- sinus: incomplete tract
Cysts are the most common, outnumbering fistulas and sinuses ~2:1 . Among fistulae and sinuses, the order prevalence is thought to be: external draining sinus > complete fistula > internal draining sinus ; although some anomalies can occur in combination.
The full list of branchial anomalies includes:
- first branchial cleft anomalies (5-8%) : seen above the level of the mandible near the external auditory canal within or close to the parotid gland.
- first branchial cleft cyst
- first branchial cleft fistula
- first branchial cleft sinus
- second branchial cleft anomalies (commonest by far: 90-95%) : between the level of the mandible angle and the carotid bifurcation, deeper than the platysma and superficial layer of deep cervical fascia
- second branchial cleft cyst
- second branchial cleft fistula
- second branchial cleft sinus
- third branchial cleft anomalies (rare): infrahyoid neck
- third branchial cleft cyst
- third branchial cleft fistula
- third branchial cleft sinus
- fourth branchial cleft anomalies (rare): infrahyoid neck, usually adjacent to the thyroid gland
- fourth branchial cleft cyst
- fourth branchial cleft fistula
- fourth branchial cleft sinus
- the fifth cleft does not give rise to the cervical sinus of His which is part of the reason that there are no fifth branchial cleft anomalies
The 3 and 4 branchial arches tend to be very close and therefore the distinction between these two cleft anomalies can be difficult on imaging .
Differential diagnosis
- Paramedian thyroglossal duct cysts (usually branchial cleft cysts are well away from the midline)
- thyroid nodules and cysts
- necrotic lymph node metastases (e.g. from squamous cell and papillary thyroid carcinomas)
- infectious adenitis (e.g. tuberculosis)
- vascular lesion on non-enhanced CT images (e.g. mycotic aneurysm)
- lymphatic malformations
- neurogenic tumors with cystic degeneration (e.g. schwannomas)
- cervical dermoid cysts
Siehe auch:
- Mediastinum
- eingeschmolzene Lymphknotenmetastasen
- Schwannom
- zystische Lymphknoten
- Schilddrüse
- Neurofibrom
- mykotisches (infiziertes) Aneurysma
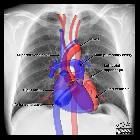
- Aortenbogen
- papilläres Schilddrüsenkarzinom
- Ductus thyreoglossus Zyste
- lymphoepitheliale Zyste der Glandula parotis
- zervikale bronchogene Zyste
- benignes Ganglioneurom
- zystische Formation am Hals
- Zyste oder Fistel des zweiten Kiemenbogens
- tuberkulöse Halslymphknoten
- zervikaler Abszess
- Halsfistel
- Zyste oder Fistel des vierten Kiemenbogens
- Kiemenbogen
- Zyste oder Fistel des ersten Kiemenbogens
- Zyste dorsal der Schilddrüse
- Zyste oder Fistel des dritten Kiemenbogens
und weiter:

 Assoziationen und Differentialdiagnosen zu Kiemenbogenzyste:
Assoziationen und Differentialdiagnosen zu Kiemenbogenzyste: