Esophageal perforation



























Esophageal perforation is a rare but serious medical emergency with a very high mortality rate, especially if the diagnosis is delayed.
Epidemiology
Most patients are in their sixties with a slight male predominance .
Clinical presentation
If a perforation is not detected during the procedure or operation, the patient may present with neck, chest or epigastric pain, dysphagia or dyspnea although symptoms asides from chest pain (present in 70%) are quite variable . Subcutaneous emphysema may also be present . There is risk of bleeding and infection .
Pathology
The lack of a serosal layer may make the esophagus more susceptible to injury than other parts of the gastrointestinal tract .
Etiology
- iatrogenic
- post instrumentation or post thoracic surgery (most common ~80% of cases)
- complication of acute radiation-induced esophagitis
- trauma: both blunt (crush-type injury) and penetrating
- occurs in <0.1% of blunt chest trauma
- foreign body ingestion
- corrosive material ingestion
- esophageal cancer
- spontaneous rupture post vomiting (Boerhaave syndrome)
Radiographic features
Plain radiograph
Possible clues on chest radiographs include:
- pneumomediastinum, abnormal cardiomediastinal contour, pneumothorax and pleural effusion are all features, although non-specific, for esophageal perforation
- widening of the mediastinal shadow: non-specific on its own
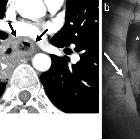
Fluoroscopy
- most sensitive within the first 24 hours
- patient examined semi-supine (~20 degrees) on the fluoroscopy table
- a low-osmolar water-soluble agent should be used initially as barium can cause mediastinitis
- esophageal perforation may be represented as mucosal irregularity or extraluminal oral contrast leak
- some authors suggest the use of small amounts of low or high concentrations of barium if no leak is evident on initial screening with water-soluble contrast
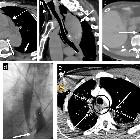
CT
The role of CT is usually to look for stigmata of perforation when fluoroscopy is equivocal, and there is persisting suspicion of perforation. These include:
- extraluminal gas locules in the mediastinum or abdominal cavity, adjacent to the esophagus are highly suggestive
- pleural or mediastinal fluid
- pneumomediastinum or pneumothorax
- pericardial or pleural effusions can be seen
Water-soluble oral contrast can be administered 20 minutes before scanning to demonstrate extraluminal contrast leak. Intravenous contrast is usually administered to delineate the esophageal wall (25 - 60-second delay) .
Treatment and prognosis
There is a high mortality rate, estimated between 25 to 50% in some series and this is significantly increased if the diagnosis is delayed beyond 24 hours .
The rarity of this condition means that treatment is not well established and options include surgical or endoscopic management vs. medical management .
Complications
- acute mediastinitis
- esophagopleural fistula
- pneumonia
- empyema
- sepsis
Siehe auch:
- Ösophaguskarzinom
- Boerhaave-Syndrom
- ösophagotracheale Fistel
- Ösophagusstents
- scheinbares zweites Lumen des oberen Ösophagus
- Ösophagusruptur
- ösophagobronchiale Fistel
- intramurale Dissektion des Ösophagus
- Ösophagusperforation durch Hühnerknochen
und weiter:

 Assoziationen und Differentialdiagnosen zu Ösophagusperforation:
Assoziationen und Differentialdiagnosen zu Ösophagusperforation:





