gastric cancer















































































Gastric adenocarcinoma, commonly, although erroneously, referred to as gastric cancer, refers to a primary malignancy arising from the gastric epithelium. It is the most common gastric malignancy. It is the third most common GI malignancy following colon and pancreatic carcinoma.
Epidemiology
Gastric cancer is rare before the age of 40, but its incidence steadily climbs after that and peaks in the seventh decade of life (from 50 to 70 years) with males predominating at 2:1 . The median age at diagnosis of gastric cancer in the United States is 70 years for males and 74 years for females.
Clinical presentation
It often produces no specific symptoms when it is superficial and potentially surgically curable, although up to 50% of patients may have nonspecific gastrointestinal complaints such as dyspepsia .
Patients may present with anorexia and weight loss (95%) as well as abdominal pain that is vague and insidious in nature. Nausea, vomiting, and early satiety may occur with bulky tumors that obstruct the gastrointestinal lumen or infiltrative lesions that impair stomach distension .
Several nodal metastases with eponymous names associated with gastric cancer have been described:
Pathology
Adenocarcinoma is by far the most common gastric malignancy, representing over 95% of malignant tumors of the stomach .
Etiology
Gastric cancer continues to be one of the leading causes of cancer-related death. A significant development in the epidemiology of gastric carcinoma has been the recognition of the association with Helicobacter pylori infection. Most gastric cancers occur sporadically, whereas 8-10% have an inherited genetic component.
Risk factors
- pernicious anemia
- adenomatous gastric polyps
- atrophic gastritis
- Billroth II partial gastrectomy for benign disease (e.g. peptic ulcer disease)
- reflux of bile and pancreatic juice as thought to be carcinogenic
- type A blood group
- smoking
Radiographic features
Endoscopy is regarded as the most sensitive and specific diagnostic method in patients suspected of harboring gastric cancer. Endoscopy allows direct visualization of tumor location, the extent of mucosal involvement, and biopsy (or cytologic brushings) for tissue diagnosis . But radiological methods are often the initial examination that raises suspicion for gastric carcinoma, besides being used in the staging of the disease.
Fluoroscopy
Early gastric cancer (elevated, superficial, shallow):
- type I: elevated lesion, protrudes >5 mm into the lumen (polypoid)
- type II: superficial lesion (plaque-like, mucosal nodularity, ulceration)
- type III: shallow, irregular ulcer crater with adjacent nodular mucosa and clubbing/fusion/amputation of radiation folds
Advanced gastric cancer:
- polypoid cancer can be lobulated or fungating
- lesion on a dependent or posterior wall; filling defect in barium pool
- lesion on non-dependent or anterior wall; etched in white by a thin layer of barium trapped between edge of mass and adjacent mucosa
- ulcerated carcinoma (penetrating cancer): 70% of all gastric cancers
Ultrasound
Not useful, unless a large epigastric mass is present or on endoscopic ultrasound study.
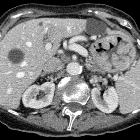
CT
CT is currently the staging modality of choice because it can help identify the primary tumor, assess for the local spread, and detect nodal involvement and distant metastases .
Demonstration of lesions facilitated by negative contrast agents (water or gas):
- a polypoid mass with or without ulceration
- focal wall thickening with mucosal irregularity or focal infiltration of the wall
- ulceration: gas-filled ulcer crater within the mass
- infiltrating carcinoma: wall thickening and loss of normal rugal fold pattern
Calcifications are rare but when present, they are usually mucinous adenocarcinoma.
Treatment and prognosis
It is an aggressive tumor with a 5-year survival rate of less than 20%. Prognosis is correlated to the stage of the tumor at presentation. Therefore, accurate staging of gastric cancer is essential because surgical resection is the treatment for localized disease .
Complications
- perforation with peritonitis: rare (thought to occur in ~2% of cases)
Differential diagnosis
The imaging differential can be broad and includes:
- gastric lymphoma
- gastric metastasis
- gastric stromal tumor (GIST)
- carcinoid tumor
- gastritis
- benign gastric (peptic) ulcer
- Menetrier disease
- secondary changes from pancreatitis (from extrinsic inflammatory change)
Siehe auch:
- Pankreatitis
- Magenulkus
- Knochenmetastasen Magenkarzinom
- gastrointestinaler Stromatumor des Magens
- Lymphom des Magens
- Morbus Ménétrier
- Laurén-Klassifikation
- Adenom des Magens
- szirrhöses Magenkarzinom
- Magenkarzinom Staging
und weiter:
- verdickte Magenwand
- Kerley-Linien
- Achalasie
- Pseudoachalasie
- linitis plastica
- Hypomotile Achalasie
- Leiomyom des Magens
- cancer
- Krukenberg-Tumor
- Magenperforation
- hereditary non-polyposis colorectal cancer
- metastases to the breast
- intramuskuläre Metastasen
- Magenneoplasien
- Hypermotile Achalasie
- MALT-Lymphom des Magens
- maligne Magenausgangsstenose
- neuroendokriner Tumor des Magens
- CA 19-9 elevation
- Klassifikation nach Laurén
- late recurrence from gastric cancer
- Lebermetastasen bei Magenkarzinom
- maligne Magentumoren
- Metastasen in der Cervix uteri
- Polypen des Magens
- Lungenmetastasen bei Magenkarzinom
- Magenkarzinom bei Kindern
- perforiertes Magenkarzinom

 Assoziationen und Differentialdiagnosen zu Adenokarzinom des Magens:
Assoziationen und Differentialdiagnosen zu Adenokarzinom des Magens: