Limbische Enzephalitis









Autoimmune encephalitis, also known as autoimmune limbic encephalitis, is an antibody-mediated brain inflammatory process, typically involving the limbic system, although all parts of the brain can be involved.
Autoimmune encephalitis can be divided broadly into two groups, based on whether or not antibodies are the result of an underlying tumor:
- paraneoplastic limbic encephalitis: usually antibodies are against intracellular antigens, poor response to immunotherapy
- non-neoplastic autoimmune limbic encephalitis: antibodies are against extracellular antigens, usually with a reversible neuronal dysfunction and better outcomes
Terminology
Unfortunately, there is considerable heterogeneity in how the term limbic encephalitis is used. Most authors limit the term to autoimmune limbic encephalitis, including both paraneoplastic and non-paraneoplastic causes. Some, however, include viral encephalitides (especially HSV encephalitis) under the broad term limbic encephalitis.
For the purpose of this article, we will restrict the term to autoimmune encephalitis, both paraneoplastic and non-paraneoplastic causes. HSV encephalitis is discussed separately.
Epidemiology
The epidemiology of tumor-related autoimmune encephalitis mimics that of the underlying malignancy.
Those with non-tumor related autoimmune encephalitis have a variable epidemiology but are mostly young patients with a female predilection .
In approximately 60% of cases, antineuronal antibodies are present such as the anti-Hu antibody in small cell lung cancer, the anti-Ta antibody in testicular cancers, anti-NMDA NR1 in ovarian teratomas or anti-NMDA NR2 in SLE patients.
Clinical presentation
Clinical presentation is variable but typically is gradual with short-term memory loss (anterograde memory impairment) and mental status changes. Psychiatric symptoms, including psychosis, depression and behavior disorder, have also been reported in over half of cases . The presence of psychiatric symptoms is particularly helpful in distinguishing limbic encephalitis from herpetic encephalitis, which otherwise can present similarly, albeit usually more acutely .
Seizures and fever are also encountered with some frequency .
Pathology
Autoimmune encephalitis can be divided according to the presence or absence of an underlying tumor, or on the type of antibody responsible.
Associated tumors
Causes of paraneoplastic autoimmune encephalitis include :
- small cell carcinoma of the lung (classic cause): anti-Hu antibodies
- testicular germ cell tumor: anti-Ta antibodies
- thymic tumors
- breast cancer
- ovarian tumors (e.g. ovarian carcinoma and ovarian teratoma)
- hematological malignancies (e.g. Hodgkin lymphoma)
- gastrointestinal malignancies
- neuroblastoma
Causes of non-paraneoplastic autoimmune encephalitis include:
- voltage-gated potassium channel (VGKC) antibody encephalitis
- anti N-methyl-D-aspartic acid (NMDA) receptor encephalitis
- systemic autoimmune conditions, e.g. systemic lupus erythematosus (SLE)
Specific antibodies
Another way of dividing autoimmune encephalitis is on the grounds of whether the antibodies are against intracellular antigens or cell surface antigens. The antibodies, in turn, correlate both to an underlying cause and pattern of involvement . As a general rule, antibodies targeted to intracellular antigens are more frequently associated with an underlying tumor .
- group I - antibodies to intracellular antigens
- anti-Hu antibodies
- most common
- small cell carcinoma of the lung in 75% of cases
- anti-Hu syndrome consists of paraneoplastic encephalomyelitis, paraneoplastic sub-acute sensory neuropathy, and paraneoplastic cerebellar degeneration
- anti-Ma/Ta antibodies
- better prognosis than anti-Hu
- testicular tumors
- diencephalic and brainstem involvement more common
- ophthalmoplegia is common
- anti-CV2 antibodies
- small cell carcinoma of the lung and malignant thymoma
- involvement of the striatum prominent
- choreiform movement disorders common
- anti-GAD (glutamic acid decarboxylase) antibodies
- usually not associated with tumors
- usually classical limbic involvement with prominent seizures and stiff person syndrome
- anti-amphiphysin antibodies
- small cell carcinoma of the lung and breast cancer
- myelopathy, myoclonus and stiff person syndrome
- anti-Ri antibodies
- small cell carcinoma of the lung and breast cancer
- brain stem involvement
- opsoclonus-myoclonus syndrome
- anti-Yo antibodies
- ovarian cancer and breast cancer
- typically presents with paraneoplastic cerebellar degeneration
- anti-Hu antibodies
- group II - antibodies to surface antigens
- anti-NMDA antibodies
- common
- usually in children and young women with no underlying tumor
- older patients may have underlying tumors (e.g. ovarian teratoma)
- typically present with psychiatric symptoms
- mild or often absent imaging changes
- anti-VGKC (voltage-gated potassium channel) antibodies
- common
- classic features of "limbic encephalitis" with prominent seizures
- extra-limbic involvement very uncommon
- anti-GABA (gamma-aminobutyric acid) antibodies
- similar to VGKC but less common
- two subtypes:
- GABA-A
- frequent extralimbic involvement
- GABA-B
- not infrequent underlying cancer (pulmonary neuroendocrine tumors)
- GABA-A
- anti-AMPA (α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid) antibodies
- predominantly psychiatric symptoms
- imaging changes limited to the hippocampi
- anti-D2 dopamine antibodies
- basal ganglia encephalitis
- anti-GlyR1 (glyoxylate reductase) antibodies
- stiff leg syndrome or stiff person syndrome, or progressive encephalomyelitis with rigidity and myoclonus
- anti-mGluR1(metabotropic glutamate receptor) antibodies
- lymphoma with cerebellar ataxia
- anti-mGluR5 antibodies
- associated with Ophelia syndrome
- anti-GluR3 (glutamate receptor) antibodies
- associated with Rasmussen encephalitis
- anti-NMDA antibodies
Radiographic features
MRI
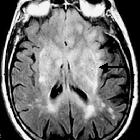
Many cases have no imaging findings, especially early in the course of the disease. Having said that, MRI with contrast is considered the most sensitive imaging modality, and findings are present in over half of individuals .
As the older term limbic encephalitis implies, the most common location of involvement is the mesial temporal lobes and limbic systems, typically manifested by cortical thickening and increased T2/FLAIR signal intensity of these regions. Bilateral involvement is most common (60%), although often asymmetric . The lateral temporal lobe and insula are less commonly involved, whereas the basal ganglia, in contrast, are frequently involved, helpful in distinguishing it from HSV encephalitis which characteristically spares the basal ganglia . Although far less common, essentially any part of the central nervous system can be involved .
Patchy areas of enhancement can be seen.
True diffusion restriction (i.e. low ADC values) and hemorrhage are not common and suggest alternative diagnoses.
The presence of hemorrhage on susceptibility-weighted images is in favor of other diagnoses such herpes simplex encephalitis which has otherwise very similar imaging appearance to limbic encephalitis.
Nuclear medicine
PET-CT may show increased FDG uptake .
Differential diagnosis
General imaging differential considerations include:
- herpes simplex encephalitis
- acute, often dramatic time course
- fever
- psychiatric symptoms uncommon
- basal ganglia spared
- status epilepticus
- acute, often dramatic time course
- tumor
- low-grade astrocytoma
- if localized to the temporal lobe, appearances can be very similar
- gliomatosis cerebri
- diffuse T2 hyperintensity involving multiple contiguous lobes
- no predilection for the limbic system
- low-grade astrocytoma
- neurosyphilis
- Hashimoto encephalopathy
Siehe auch:
- Gliomatosis cerebri
- Astrozytom
- Herpesenzephalitis
- Virusenzephalitis
- Enzephalitis
- paraneoplastisches Syndrom
und weiter:

 Assoziationen und Differentialdiagnosen zu Limbische Enzephalitis:
Assoziationen und Differentialdiagnosen zu Limbische Enzephalitis: