Normaldruckhydrozephalus










Normal-pressure hydrocephalus remains a controversial entity with often ambiguous imaging findings. It is classically characterized by the triad of gait apraxia/ataxia, urinary incontinence, and dementia, although not all patients with the condition have all three.
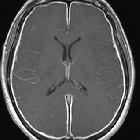
On imaging, it can be characterized both on CT and MRI by enlarged lateral and third ventricles out of proportion to the cortical sulcal enlargement.
This article is focused on idiopathic cases. For a discussion of secondary causes of communicating hydrocephalus, please refer to the article hydrocephalus.
Terminology
It is important to note that there are many causes of communicating hydrocephalus without elevated opening CSF pressures, such as trauma, prior subarachnoid hemorrhage, and meningitis. This is sometimes confusingly referred to as secondary normal pressure hydrocephalus . Most clinicians will assume that one is referring to idiopathic normal pressure hydrocephalus if no qualifier is used.
Epidemiology
The majority of cases are idiopathic. The incidence is much higher in elderly populations. Exact epidemiology is difficult to establish, as the diagnosis is often not made in nursing home patients for the following reasons:
- approximately 20% of patients in nursing homes have gait impairment
- approximately 10% of these patients also have dementia
- 15% have incontinence
A large study in Norway found a striking increase in incidence with increasing age:
- 3.3 per 100,000 for people 50 to 59 years of age
- 49.3 per 100,000 for people 60 to 69 years of age
- 181.7 per 100,000 for people 70 to 79 years of age
Clinical presentation
The classical clinical findings of normal pressure hydrocephalus are
- urinary incontinence
- deterioration in cognition (dementia)
- gait disturbances
These can be remembered with the unkind mnemonic Wet, Wacky, and Wobbly.
As the name suggests, mean CSF opening pressure is within the normal range (<18 cmH2O or 13 mmHg) .
A classic neurological sign in NPH is magnetic gait, where the patients' feet appear to be magnetically attached to the floor.
Pathology
The underlying cause remains controversial. One theory is that the condition is an obstructive type of communicating hydrocephalus due to reduced CSF resorption. A second theory suggests it results from weakening of the ventricular wall due to periventricular white matter ischemic damage . The periventricular white matter ischemic change has also been hypothesized to slow the flow of CSF through the extracellular spaces, resulting in a "back-pressure" effect, leading to ventricular enlargement.
Shearing forces are exerted on the periventricular white matter as the ventricles enlarge. As the corticospinal tracts to the legs run medially, these tangential shearing forces cause gait disturbance.
Radiographic features
CT
Although CT is able to visualize the anatomical changes, it is inferior to MRI.
MRI
MRI is the best modality to image anatomical changes and can further support the diagnosis with CSF flow studies and magnetic resonance spectroscopy.
Morphological changes
- ventriculomegaly
- increased Evans' index >0.3
- widening of the temporal horns of the lateral ventricles >6 mm
- acute callosal angle
- upward bowing of the corpus callosum
- disproportionate changes in subarachnoid spaces
- dilated Sylvian fissures
- tight high convexity (narrow sulci and subarachnoid spaces at the vertex and medial/parafalcine region)
- cingulate sulcus sign: posterior half of cingulate sulcus is narrower than the anterior half
- focal/isolated dilation of sulci over the medial surface or convexity (sometimes called transport sulci)
The combination of ventriculomegaly, Sylvian fissure widening, and crowding at the vertex has been termed disproportionately enlarged subarachnoid space hydrocephalus (DESH), reflecting disproportionality between the superior and inferior CSF spaces . The finding of DESH without neurologic symptoms has been termed asymptomatic ventriculomegaly with features of idiopathic normal pressure hydrocephalus on MRI (AVIM) . It is felt by some authors that AVIM is actually a pre-clinical form of iNPH .
Brain composition changes
Periventricular hypodensity (on CT) or high T2-FLAIR signal (on MRI) is supportive of changes in brain water content seen in NPH, but these findings can also be seen with microvascular ischemic changes or demyelination .
CSF flow changes
Although prominent aqueductal flow void due to increased CSF velocity across the aqueduct is often seen in patients with NPH - best seen on T2 and PD spin-echo sequences - it is no longer considered a useful sign, as in modern higher field strength MRI machines aqueductal CSF flow void is present in most of the normal subjects. Additionally, it is highly sequence-specific.
There is, however, a well-established correlation between higher flow velocities and the favorable outcome after ventriculoperitoneal (VP) shunting; hence, quantitative (rather than qualitative) methods have been developed which can be useful not only in patient selection for shunting but also in diagnosis and predicting prognosis
- CSF flow studies
- increased aqueductal CSF stroke volume
- aqueductal CSF stroke volume is the average volume of CSF flowing through the cerebral aqueduct during both systole and diastole
- increased aqueductal peak velocity
- various publications have set various normal and abnormal ranges
- flow rate of >24.5 mL/min 95% specific for NPH
- stroke volume of ≥42 μL shown in one paper to predict a good response to shunting , however, a more recent paper has cast serious doubt on the usefulness of aqueduct stroke volume in patient selection for VP shunting
- stroke volume upper limit is now suggested to be variable between institutions due to intrinsic scanner differences; thus each center should obtain their own "normal values", with the upper limit being suggested as two times the normal value
- studies have shown that aqueductal stroke volume decreases later in the disease process despite clinical progression
- this has been theorized to be caused by cerebral atrophy, which indicates that the patient is unlikely to respond to shunt surgery
- increased aqueductal CSF stroke volume
MR spectroscopy
MRS has not been shown to have any added value for differentiating idiopathic NPH from other types of dementia, nor does it help in patient selection for VP shunting .
Nuclear medicine
Nuclear medicine is less important in diagnosing NPH. Some of the features described are
- early detection of the radiotracer into lateral ventricles giving a heart-shaped appearance of lateral ventricles rather than a normal trident pattern
- persistence of radiopharmaceutical beyond 24-48 hours due to impaired absorption
- radiotracer does not extend to the superior aspect of convexities of lateral ventricles
- retrograde CSF flow into lateral ventricles
Treatment and prognosis
Treatment of normal pressure hydrocephalus, once the diagnosis is established, is with CSF shunting, usually a ventriculoperitoneal shunt (VP shunt). The challenge is identifying those patients who will benefit from shunting. Favorable prognostic factors include
- short duration of presurgical symptoms (less than 6 months)
- onset of gait disturbance before dementia
- temporary symptom relief from a CSF tap test (removal of 40ml of CSF via lumbar puncture)
- absence of significant cerebral vascular disease
- presence of an aqueductal flow void on T2 imaging
History and etymology
It is thought to have been initially described by Colombian neurosurgeon Salomón Hakim and R D Adams in 1965, although it may actually have been described earlier under a different name by McHugh .
Differential diagnosis
The possible imaging differential spectrum includes:
- normal aging brain
- Alzheimer dementia: may show greater dilatation of perihippocampal fissures
- obstructive hydrocephalus: due to mass lesion (e.g. pineal region, tectal plate, midbrain)
- Lewy body dementia: visual hallucinations and delusions are more prominent
- Parkinson disease: unilateral symptoms are important
- AIDS-dementia complex: positive HIV serology
Siehe auch:
- Subarachnoidalblutung
- Corpus-callosum-Winkel
- MR spectroscopy
- Corpus callosum
- Meningitis
- Seitenventrikel
- Verschlusshydrocephalus
- ventrikuloperitonealer Shunt
- ventriculomegaly
- Evans Index
- Hakim Trias
- Morbus Alzheimer
und weiter:

 Assoziationen und Differentialdiagnosen zu Normaldruckhydrozephalus:
Assoziationen und Differentialdiagnosen zu Normaldruckhydrozephalus: