obstructive hydrocephalus




















Obstructive hydrocephalus is a term usually used to denote obstructive non-communicating hydrocephalus.
It is actually a term that causes confusion as used in the above sense implies that communicating hydrocephalus does not have an obstruction to CSF flow/absorption; this is not true as the majority of cases of communicating hydrocephalus have obstruction to CSF flow through the subarachnoid space or impaired absorption at the arachnoid granulations.
For a discussion of this terminology, please refer to the most general article on hydrocephalus.
The remainder of this article pertains to the commonly used meaning of obstructive hydrocephalus, namely obstructive non-communicating hydrocephalus.
Epidemiology
The demographics of affected patients will depend on the underlying causes, which include:
- congenital aqueduct stenosis
- obstructing tumor or mass (e.g. tectal plate glioma, colloid cyst)
Clinical presentation
As is the case with most mass effect conditions affecting the brain, the presentation will vary dramatically depending on the speed of onset.
In acute obstructive hydrocephalus, as is the case with a colloid cyst obstructing the foramina of Monro, a sudden increase in intraventricular pressure can lead to rapid loss of consciousness and even death.
In other patients where the obstruction is incomplete or gradual (e.g. aqueduct stenosis), there may be almost no symptoms despite massive dilatation of the ventricles.
Overall the presentation will depend on the presence of raised intracranial pressure that has the usual constellation of symptoms including headaches, made worse with stooping or straining, nausea, and vomiting. Papilledema may be evident .
In children whose cranial sutures have yet to fuse, there is a rapid enlargement of the head circumference .
Radiographic features
Both CT and MRI (and ultrasound in the neonatal period) can demonstrate most of the features, although the underlying cause may be more or less easily discernible (e.g. a web across the aqueduct causing aqueduct stenosis will only be visible on dedicated high-resolution MRI images).
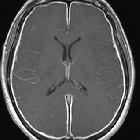
Acute obstructive hydrocephalus
An important caveat to be aware of is that in acute obstructive hydrocephalus in young patients only minor ventriculomegaly may be visible despite the significant elevation of intracranial pressure.
If previous films are available, they are probably the most reliable way of identifying early hydrocephalus. Features that are helpful in making the diagnosis of acute obstructive hydrocephalus include :
- lateral ventricles
- enlargement of the temporal horns (best indicator)
- transependymal edema, or periventricular oozing, may be visible as high T2 signal on MRI or low-density change on CT around the margins of the ventricles, and should not be confused with white matter change of chronic small vessel ischemia.
- third ventricle
- outward bowing of the lateral walls
- inferior bowing of the floor
- fourth ventricle
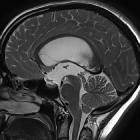
Chronic non-communicating obstructive hydrocephalus
Non-communicating obstructive hydrocephalus (often merely referred to as obstructive hydrocephalus) is usually a relatively straightforward diagnosis to make on imaging. Over time, the portions of the ventricular system upstream from the obstruction gradually enlarge compressing and thinning the overlying cortex.
Features of long-standing non-communicating obstructive hydrocephalus (at the level of the aqueduct of Sylvius or below) include :
- marked dilatation of the ventricles, especially the lateral and third ventricles
- thinned and elevated corpus callosum
- fenestration of the septum pellucidum
- depression of the fornices
- the floor of the 3 ventricle is displaced inferiorly, abutting the skull base, obliterating the suprasellar cistern
- outward bowing (ballooning) of the recesses of the third ventricle (infundibular, optic and pineal recesses)
- ballooning of the suprapineal recess
Treatment and prognosis
Treatment depends on the cause and location of the obstruction. In some patients with temporary obstruction (such as with subarachnoid hemorrhage), temporary CSF diversion is sufficient (e.g. via an external ventricular drain (EVD)). Similarly, if the cause is mechanical, it may be possible to resect the mass (e.g. colloid cyst).
In many cases, obstruction is permanent or unable to be directly treated (e.g. most tectal gliomas), and as such permanent CSF diversion may be required. Treatment options include:
- shunting, most commonly with a VP shunt
- third ventriculostomy is useful in patients with non-communicating obstructive hydrocephalus at or below the level of the aqueduct of Sylvius
Siehe auch:
- Hydrocephalus
- Subarachnoidalblutung
- Corpus callosum
- Normaldruckhydrozephalus
- Meningitis
- dritter Ventrikel
- Tectumgliom
- Seitenventrikel
- Aquäduktstenose
- vierter Ventrikel
- ventrikuloperitonealer Shunt
- transependymales Ödem
- hydrocephalus versus atrophy
- third ventriculostomy
- Liquorzirkulationsstörung
- pädiatrische Erkrankungen des Liquorsystems
- Stenose des Foramen Monroi
- Magendie
- Luschka
und weiter:
- Xanthogranulome des Plexus choroideus
- Basiläre Impression
- intraventrikuläre Blutung
- Hypophysenadenom
- Pineozytom
- Kleinhirnblutung
- juvenile maligne Osteopetrose
- Kolloidzyste des dritten Ventrikels
- Morbus Alexander
- aqueduct of Sylvius
- kongenitale Aquäduktstenose
- Papillärer Tumor der Pinealisregion
- Apoplex der Glandula pinealis
- transcallosal approach
- Pinealisinfarkt
- tuberkulöse Meningitis
- Tectum mesencephali
- PICA infarct with hydrocephalus
- erweiterte Ventrikel
- atrial diverticulum secondary to a colloid cyst of the third ventricle
- supraselläre Arachnoidalzyste
- Foramen interventriculare Monroi
- atrial diverticulum
- Arachnoidalzysten der hinteren Schädelgrube mit Hydrozephalus
- Hydranenzephalie

 Assoziationen und Differentialdiagnosen zu Verschlusshydrocephalus:
Assoziationen und Differentialdiagnosen zu Verschlusshydrocephalus: