Aquäduktstenose











Aqueductal stenosis (AS) is the most common cause of congenital obstructive hydrocephalus, but can also be seen in adults as an acquired abnormality.
Epidemiology
Congenital aqueductal stenosis has an estimated incidence of ~1:5000 births although the reported range varies greatly (3.7:1,000,000 to 1:2000) . Rarely it may be inherited in an X-linked recessive manner (Bickers-Adams-Edwards syndrome) .
In adults, as an acquired abnormality, AS has different etiologies and thus different demographics related to them.
Clinical presentation
The clinical presentation depends on the severity and age of presentation as well as whether or not it is X-linked. In the infant enlarging head size, bulging fontanelles and gaping cranial sutures are seen. Setting sun phenomenon may also be present. In X-linked form (Bickers-Adams-Edwards syndrome) which is associated with profound intellectual disability, clinical assessment would reveal bilateral adducted thumbs.
The usual symptoms and signs of raised intracranial pressure and chronic hydrocephalus may also be present, including headache, vomiting, decreased conscious state .
Pathology
- congenital
- aqueductal webs or diaphragms
- gliosis
- acquired
- extrinsic compression
- intrinsic
- infection: meningitis/ventriculitis
- subarachnoid hemorrhage (SAH)
Radiographic features
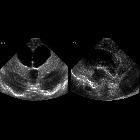
Ultrasound
An antenatal exam can show features of fetal hydrocephalus with a near-normal posterior fossa. There can be secondary thinning of the cortical mantle as well as secondary macrocephaly.
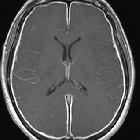
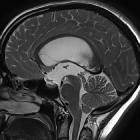
MRI
Better delineates the extent of obstructive hydrocephalus, with an enlargement (often marked) of the lateral and third ventricles. The aqueduct may show funnelling superiorly. The 4 ventricle is not dilated. In cases of secondary obstruction, the underlying abnormality may also be evident (e.g. web, tumor).
- sagittal T2: the absence of flow-void signal intensity at the aqueductal level has been suggested as a sign of aqueductal stenosis
- sagittal CISS: best demonstrates obstructing web
- CSF flow study: decreased aqueductal stroke volume and peak systolic velocity
Treatment and prognosis
Treatment is often either with a third ventriculostomy or VP shunting. There is a small recurrence risk (~4%) for congenital cases even when it is not X linked.
Siehe auch:
- Hydrocephalus
- Subarachnoidalblutung
- Meningitis
- Tumoren der Pinealisregion
- Tectumgliom
- Makrozephalie
- Tumoren der hinteren Schädelgrube
- Verschlusshydrocephalus
- Ventrikulitis
- intrakranielle vaskuläre Malformationen
- third ventriculostomy
- kongenitale Aquäduktstenose
- Webstenose des Aquädukts
- Bickers-Adams-Edwards syndrome
- kongenitaler Hydrozephalus
- erworbene Aquädukstenose
- Setting sun phenomenon
und weiter:

 Assoziationen und Differentialdiagnosen zu Aquäduktstenose:
Assoziationen und Differentialdiagnosen zu Aquäduktstenose: