Tumoren der hinteren Schädelgrube

Als
Zufallsbefund in der Magnetresonanztomographie entdecktes Lipom der Vierhügelplatte bei eine 69-jährigen. Links in T2 mäßig signalreich, in der Mitte in T1 KM (auch ohne) und rechts in FLAIR sehr signalreich.

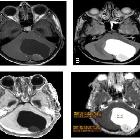
Patterns of
relapse in primary central nervous system lymphoma: inferences regarding the role of the neuro-vascular unit and monoclonal antibodies in treating occult CNS disease. Case 4; Axial T1 WI post contrast imaging at initial presentation (a, b) and relapse (c, d). At initial presentation there is a solitary right cerebellar lesion (a) with normal supra-tentorial compartment (b). After 10 months of high-dose MTX treatment, relapse was noted in the splenium of the CC with extension to the periventricular white matter (d) with no evidence of residual disease in the cerebellum (c)

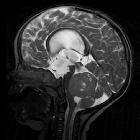
Brain MRI
showing primary central nervous system B-cell non-Hodgkin lymphoma of the sella turcica and hypothalamus, continuing to the tectum.

Hemangioblastoma
(central nervous system) • Posterior fossa hemangioblastoma - Ganzer Fall bei Radiopaedia

Posterior
fossa tumors • Posterior fossa ependymoma - Ganzer Fall bei Radiopaedia

Pilocytic
astrocytoma • Pilocytic astrocytoma - Ganzer Fall bei Radiopaedia

Medulloblastoma
• Medulloblastoma - Ganzer Fall bei Radiopaedia

Posterior
fossa tumors • Posterior fossa ependymoma - Ganzer Fall bei Radiopaedia

Trigeminal
neuralgia and posterior fossa meningioma: case report and review of literature. Posterior fossa MR imaging: more caudal sections show contrast-enhanced lesion attached to the dura

Trigeminal
neuralgia and posterior fossa meningioma: case report and review of literature. Posterior fossa MR imaging of the right trigeminal neuralgia patient. The lesion on the right side of the V. nerve (possibly vascular structure) is visible. This structure during surgery has been found to be compatible with the superior cerebellar artery

Adult
medulloblastoma: a case report. T1W image showing hypointense left lateral posterior cranial fossa lesion as indicated by the arrow

Patterns of
relapse in primary central nervous system lymphoma: inferences regarding the role of the neuro-vascular unit and monoclonal antibodies in treating occult CNS disease. Case 3; Axial T1-weighted post contrast imaging at initial presentation (a, b), after completing therapy with HD-MTX (c) and relapse (d). Initial presentation shows a large enhancing lesion in the left frontal lobe (a) and normal cerebellum (b). Patient was in complete response after completing 1 year of HD-MTX treatment (c) with radiographic relapse in the right cerebellum, 6 years after the initial diagnosis (d)

Medulloblastoma
in an adult. The lesion showed mild contrast enhancement with heterogeneous appearance due to central cystic or necrotic areas.

Medulloblastoma
in an adult. The mass is moderately hyperintense on T2-weighted images. FLAIR sequence shows surrounding vasogenic oedema.

Role of
diffusion-weighted imaging in differentiation between posterior fossa brain tumors. Epidermoid cyst in 38-year-old male complaining from auditory problems. A lobulated extra-axial cystic lesion is seen in the right cerebellopontine angle (CPA) insinuating itself, compressing the pons, extending into prepontine cistern, and encasing the basilar artery. It displays low T1WI signal intensity (a) and high T2WI signal intensity cerebrospinal fluid (CSF) like (b). On FLAIR, it shows low SI (partially suppressed SI (c). It shows faint marginal enhancement on post-contrast study (d). It shows iso SI-like brain parenchyma (restricted diffusion); it does not have high CSF SI-like arachnoid cyst (e)

Role of
diffusion-weighted imaging in differentiation between posterior fossa brain tumors. Typical cerebellar (infratentorial) meningioma in female patient aged 44 years old presented with chronic headache and dizziness 4 months ago. An extra-axial space-occupying lesion (SOL) is seen in the left cerebellar hemisphere lying below and contacting the tentorium cerebelli with moderate perifocal edema, effacement of related cerebellar folia, compression of the fourth ventricle, and minimal rightward shift of midline structures. This mass displays relatively iso to low signal intensity (SI) on T1WI (a), iso SI on T2 WI (b). It shows homogeneous enhancement on post-contrast T1WI (c). It has iso SI-like brain parenchyma on apparent diffusion coefficient images (ADC) map (d)

Role of
diffusion-weighted imaging in differentiation between posterior fossa brain tumors. Typical MRI features of a medulloblastoma in a 3-year-old child who presented with chronic headache 5 months ago. a T1WI shows midline vermian hypointense mass in the posterior fossa causing anterior displacement of the fourth ventricle. b T2WI: the mass appears isointense to slightly hyperintense. Few T1WI hypointense and T2WI hyperintense foci suggestive of cystic components. c Post-contrast T1WI axial image showing intense enhancement of the mass. d Low signal on apparent diffusion coefficient images (ADC), features suggestive of restricted diffusion corresponding to hypercellularity of the mass
Role of
diffusion-weighted imaging in differentiation between posterior fossa brain tumors. Juvenile pilocytic astrocytoma in a 9-year-old boy who presented with repeated headache and vomiting. a T1-weighted (T1WI) shows intra-axial cystic space-occupying lesion (SOL) in the left cerebellar hemisphere. b T2-weighted (T2WI) showing hyperintense cystic posterior fossa mass with isointense solid mural nodule attached to the inner side of the cystic mass. Note the cystic components and relatively solid components. c Post-contrast T1WI axial image showing mildly enhancing solid components and faint enhanced cystic wall. d Apparent diffusion coefficient (ADC) map: the cystic component is bright while the solid component is relatively lower than the cystic component with slight diffusion restriction

Posterior
fossa tumors • Cerebellar metastasis - Ganzer Fall bei Radiopaedia
Posterior fossa tumor has a very different differential in an adult as opposed to a child.
Adult
- cerebellar metastases (most common)
- especially lung cancer and breast cancer
- also melanoma, thyroid malignancies, and renal cell cancer
- gastrointestinal stromal tumor (very rare)
- hemangioblastoma: most common posterior fossa primary brain tumor in adults
- astrocytomas, medulloblastomas, and ependymomas are encountered in the posterior fossa of younger adults but are rare in older adults, accounting for <1% all tumors
- posterior fossa meningioma
- lymphoma
- lipoma
- Lhermitte-Duclos disease
- medulloblastoma in adults
An important space-occupying lesion (the most common in fact) to remember is that of a stroke, which when subacute can mimic a tumor.
Child
- posterior fossa astrocytoma
- pilocytic astrocytoma: second most common (25-35%)
- brainstem glioma
- medulloblastoma: most common (30-40%)
- ependymoma
- atypical teratoid/rhabdoid tumor (AT/RT)
- hemangioblastoma (uncommon except in patients with vHL)
- teratoma (in infants)
A quick and handy mnemonic for posterior fossa tumors in children is BEAM.
Although it is true that posterior fossa tumors are much more common in children than in adults the distribution does vary with age :
- 0 to 3 years of age: supratentorial > infratentorial
- 4 to 10 years of age: infratentorial > supratentorial
- 10 to early adulthood: infratentorial = supratentorial
- adults: supratentorial > infratentorial
Overall 50-55% of all brain tumors in children are found in the posterior fossa .
Siehe auch:
- Pilozytisches Astrozytom
- Ependymom
- Teratom
- Medulloblastom
- Hämangioblastom
- Astrozytom
- Morbus Hippel-Lindau
- Apoplex
- posterior fossa astrocytoma
- Tumoren der Schädelbasis
- AV Malformation hintere Schädelgrube
- intrakranielle Lipome der hinteren Schädelgrube
- cerebellar metastases
- atypischer teratoider rhabdoider Tumor
- Hirnnervenlähmungen
- Medulloblastom bei Erwachsenen
- Meningeom der hinteren Schädelgrube
- BEAM (Merkhilfe Tumoren der hinteren Schädelgrube bei Kindern)
- primary brain tumour
- Hirnstammgliom
und weiter:

 Assoziationen und Differentialdiagnosen zu Tumoren der hinteren Schädelgrube:
Assoziationen und Differentialdiagnosen zu Tumoren der hinteren Schädelgrube:













