pituitary apoplexy

















Pituitary apoplexy is an acute clinical syndrome caused by either hemorrhagic or non-hemorrhagic necrosis of the pituitary gland. Although variable, it typically comprises headache, visual deficits, ophthalmoplegia, and altered mental status. An existing pituitary macroadenoma is usually present (60-90%), but it has occurred with healthy glands in a few isolated cases.
Epidemiology
The demographics generally follow that of pituitary macroadenomas. Additional predisposing factors include :
- medical treatment of a prolactinoma (especially with bromocriptine)
- prior irradiation of the mass
- pregnancy (Sheehan syndrome)
- cerebral angiography
- trauma and surgery
- anticoagulation therapy
- changes in intracranial pressure
Clinical presentation
As the gland suddenly enlarges it may cause compression of structures adjacent to the sella, and thus elicit a number of signs and symptoms, including :
- sudden headache
- loss of visual acuity with a chiasmal field defect
- oculomotor palsies
Also, the patient may experience a decreased level of consciousness, hypopituitarism, Addisonian crisis , and subarachnoid irritation, the latter being secondary to hemorrhage.
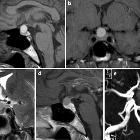
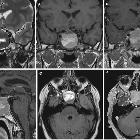
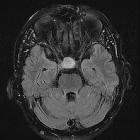
Radiographic features
General features include enlargement of the pituitary gland, with or without bleeding. Macroscopic hemorrhage is common and occurs in about 85%. It shows peripheral enhancement around a non-enhancing infarcted center. Surrounding edema may be seen in the optic tracts and chiasm.
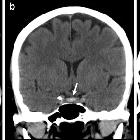
CT
Routine CT is insensitive to the diagnosis unless frank intracranial hemorrhage is present. The pituitary mass may be evident and may be hyperdense. Fluid-debris levels may also be evident.
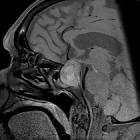
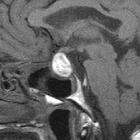
MRI
MRI typically demonstrates a pituitary region mass.
- T1: variable; in cases with hemorrhagic infarction, it is hyperintense due to blood (see aging blood on MRI)
- T2: variable signal
- T1 C+ (Gd): enhancement variable; usually peripheral and may be difficult to identify due to intrinsic high T1 signal
- DWI: restricted diffusion may be present in solid infarcted components
Treatment and prognosis
If prompt neurosurgical intervention with the transsphenoidal approach is available to decompress the gland, prognosis is good. Without surgery, the majority of the patients die. Conservative management may be chosen in selected cases. Pituitary apoplexy is usually associated with irreversible hypopituitarism and often ophthalmoplegia and visual loss .
Differential diagnosis
The differential is broadly that of a pituitary region mass, but as these patients present acutely with acute or subacute blood products, it can usually be limited to pituitary region masses with intrinsic high T1 signal.
- necrotic/hemorrhagic pituitary macroadenoma
- appearances are the same, but patients do not present acutely
- whether or not the term apoplexy can be used in subacute presentations is debatable
- craniopharyngioma (adamantinomatous type)
- calcification in 90%
- usually in children
- usually not acute presentation
- Rathke cleft cyst
- usually asymptomatic
- no associated mass
- spherical
- dermoid/teratoma
- usually have a fat component
- unless ruptured, the presentation is usually insidious
- if ruptured, locules of fat density/intensity material are often seen in the subarachnoid space
Siehe auch:
- Rathke Zyste
- Tumoren der Hypophysenregion
- Makroadenom Hypophyse
- Teratom
- Kraniopharyngeom
- thunderclap headache
- postpartum hypopituitarism
- Hypophysenischämie
- Hypophysenadenom Einblutung
- pituitary region masses with intrinsic high T1 signal
und weiter:

 Assoziationen und Differentialdiagnosen zu Apoplex der Hypophyse:
Assoziationen und Differentialdiagnosen zu Apoplex der Hypophyse: