Hypophyse

















The pituitary gland (or hypophysis cerebri), together with its connections to the hypothalamus, acts as the main endocrine interface between the central nervous system and the rest of the body.
Gross anatomy
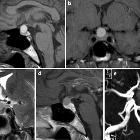
The pituitary gland sits atop the base of the skull in a concavity within the sphenoid bone called the sella turcica (pituitary fossa), immediately below the hypothalamus and optic chiasm.
The pituitary is usually divided (in practice) into anterior and posterior parts, which actually refers to groupings of four subparts :
- anterior pituitary
- pars distalis
- pars tuberalis
- pars intermedia
- posterior pituitary
- neurohypophysis
The anterior lobe of the pituitary is surrounded by a thin fibrous capsule, similar to that of salivary glands, continuous with thin septae which extend into the gland .
The pituitary fossa is surrounded by a layer of dura, continuous with the diaphragma sellae above (the dural anatomy is discussed in more detail in the pituitary fossa article). The diaphragma sellae has a variably sized opening for the infundibular stalk. Not uncommonly the diaphragma sellae is incomplete (considered a normal variant) and CSF may enter into the pituitary fossa and may give rise to the "empty sella sign" on neuroimaging.
Anterior pituitary
The anterior pituitary is by far the largest part of the gland and is responsible for synthesis and release of most pituitary hormones (with the exception of oxytocin and antidiuretic hormone (ADH) which are released by the posterior pituitary).
Pars distalis
The pars distalis is the largest part of the pituitary gland. It arises from the anterior wall of Rathke pouch. It is composed of cords of epithelial cells individually specialized to secrete trophic hormones acting on various target organs (see below).
Pars tuberalis
The pars tuberalis is the part of the adenohypophysis which surrounds the anterior aspect of the infundibular stalk.
Pars intermedia
The pars intermedia in a thin layer of epithelial cells located between pars distalis and neurohypophysis. It arises from the posterior wall of Rathke pouch and contains vestigial lumina of Rathke pouch which appears as narrow vesicles of variable length. These may give rise to Rathke cleft cysts (also known as pars intermedia cysts ).
Posterior pituitary (neurohypophysis)
The posterior pituitary (aka neurohypophysis) is a direct extension from the hypothalamus, connected to it via the infundibular stalk, which is also considered part of the neurohypophysis. The infundibulum extends from the tuber cinereum and pierces the diaphragma sella before being surrounded by the pars tuberalis.
Oxytocin and antidiuretic hormones are synthesized in the hypothalamus and travel down the stalk to be released in the posterior pituitary.
Relations
The pituitary, located within the pituitary fossa, has complex relations.
- inferiorly
- sphenoid bone (basisphenoid)
- sphenoid sinus
- superiorly
- diaphragma sellae and hypophyseal cistern
- suprasellar cistern
- laterally
- cavernous sinuses (and contents)
- anteriorly
- anterior intercavernous sinus
- anterior clinoid processes
- posteriorly
Hormone secretion and control
Anterior pituitary
The anterior pituitary secretes six hormones, each with distinct functions and target organs:
Most of the aforementioned hormones' release is controlled by releasing hormones secreted by the hypothalamus into the portal circulation. The exception is prolactin which, except during pregnancy when it too is stimulated by a releasing hormone, is tonically inhibited by prolactin inhibitory hormone (PIH) which is actually dopamine. Thus, dopamine antagonists (e.g. many antipsychotics) result in elevated prolactin levels. Conversely, prolactin secreting adenomas (prolactinomas) can be treated medically with dopamine agonists (e.g. bromocriptine and cabergoline). For a more in-depth discussion refer to elevated prolactin (differential) article.
Posterior pituitary
The posterior pituitary does not directly synthesize any hormones but rather releases oxytocin and ADH (vasopressin) which have traveled down the infundibulum in vesicles termed Herring bodies. The cell bodies reside in two hypothalamic nuclei:
- supraoptic nucleus
- paraventricular nucleus
Size and age-dependent changes
The pituitary gland volume changes depending on hormonal status, most dramatically during pregnancy when it can be markedly enlarged, sometimes mistaken for an adenoma. The size of the pituitary also changes with age.
Generally speaking, young adults have larger glands than older individuals, and hormonally active individuals (puberty/pregnancy) have the largest glands. These plump glands completely fill the pituitary fossa, and have a convex upper border, whereas older individuals will have a largely empty pituitary fossa, with a deflated and thinned gland lying on the floor of the sella.
Although one should always be wary of measurements, they can serve to quantify what may otherwise seem overly subjective impressions. These are reasonable maximal figures for the height of the gland (also see Elster's rule):
- children (<12 years): 6 mm (upper surface flat or slightly concave)
- puberty: 10 mm (upper surface convex; more striking in females)
- young adult
- male: 8 mm
- female: 9 mm
- pregnancy: 12 mm
- older adult (>50 years): gradually decreases in size
- there is a slight increase in size in the perimenopausal period for women, but still remaining smaller than a pituitary of a young woman
Blood supply
The pituitary gland has a rich blood supply, with both a portal circulation (to the anterior pituitary) and arterial supply (to the posterior pituitary and pituitary stalk) .
Arterial circulation
A rich network of small branches supplies the stalk and the posterior pituitary, with a total of six arteries described, three from above and three from below/side (from the cavernous segment of the internal carotid artery). These arteries anastomose with each other to form two networks of vessels :
Branches
- from above
- superior hypophyseal artery (from the internal carotid artery)
- infundibular artery (from the posterior communicating artery)
- prechiasmal artery (from the ophthalmic artery)
- from below/side (cavernous carotid artery)
- inferior hypophyseal artery (from the meningohypophyseal trunk)
- capsular artery
- artery of the inferior cavernous sinus
Portal circulation
The anterior pituitary receives blood which descends from the hypothalamus along the infundibulum as a portal system (venous channels connecting two capillary beds); this accounts for the typical pattern of contrast enhancement seen on dynamic MRI imaging.
The superior hypophyseal arteries give superior branches which supply the superior most infundibulum which receives axons from a number of hypothalamic nuclei. These axons release various releasing and inhibiting factors which are then taken down the infundibulum in the hypophyseal portal venous plexus, and thus delivered to the anterior pituitary where they control the release of its numerous hormones .
Venous drainage
Venous blood drains into the nearby cavernous and intercavernous sinuses.
Variant anatomy
The main variations are in size/number :
- hypoplasia
- hyperplasia: physiologic prolactin cell hyperplasia due to lactation or pregnancy and in response to end organ failure such as Addison disease, Klinefelter or Turner syndrome, or primary hypothyroidism
- partially empty sella turcica (see: empty sella sign)
- duplication
Embryology
The pituitary gland has a dual origin (ectoderm of the primitive mouth cavity and neuroectoderm of the diencephalon) which reflects the two distinct parts in the adult gland.
At approximately 24 days gestation the beginnings of the adenohypophysis and neurohypophysis begin to form as Rathke pouch, which forms as an ectodermal outpouching of stomodeum (primitive oral cavity lined by ectoderm) and the infundibulum which forms in the floor of the diencephalon (part of the neural tube).
The infundibulum grows ventrally towards the stomodeum while simultaneously Rathke pouch grows dorsally. Rathke pouch eventually loses its connection with the stomodeum and forms a discrete sac which adheres to the infundibular process. This sac differentiates to form the adenohypophysis of the pituitary: pars distalis, pars tuberalis, and pars intermedia. The distal part of the infundibulum differentiates to form the posterior pituitary (neurohypophysis) and retains the connection with the hypothalamus as the stalk.
By the sixth week, the connection with the oral cavity has been lost. If this connection persists then the structure is called a pharyngeal hypophysis, occasionally associated with nests of pituitary cells along this course, and accounting for rare macroadenomas in the nasopharynx.
Related pathology
- pituitary tumors
- pituitary apoplexy
- pituitary stalk abnormal enhancement
- Rathke cleft cyst
- craniopharyngioma
- ectopic posterior pituitary
- pituitary stalk interruption syndrome
See also

 Assoziationen und Differentialdiagnosen zu Hypophyse:
Assoziationen und Differentialdiagnosen zu Hypophyse: