Pituitary MRI (an approach)








A systematic approach to the pituitary region is crucial as small lesions can have a profound impact on the patient, and can be subtle even on high quality dedicated MRI imaging. Successful assessment of the pituitary region relies not only on a clear understanding of the local anatomy but also on the relatively wide variety of pathologies that occur in the region.
Imaging protocol
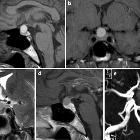
A typical targeted MRI examination of the pituitary region includes coronal and sagittal small field of view T1 and T1 post-contrast images, as well as dynamic contrast-enhanced coronal images, which are critical for the identification of small microadenomas. T2 weighted sequences are often also included, although are of relatively little-added benefit. Please, refer to the article on pituitary gland protocol (MRI) for a detailed discussion on this topic.
Normal appearance on MRI
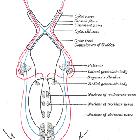
Before being able to interpret MRIs of the region it is important to understand the normal anatomy of the pituitary gland and surrounding structures:
- pituitary gland
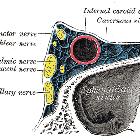
- cavernous sinus
- optic nerve/optic chiasm/optic tract
- suprasellar cistern
- third ventricle
The anterior and posterior parts of the pituitary gland are distinct on MRI. The anterior part is isointense on both T1 and T2 weighted images. The posterior pituitary has intrinsic high T1 signal and is of a hypointense signal on T2 weighted images . During the dynamic contrast-enhanced sequence, contrast can be seen to wash into the gland from the infundibulum and gradually spread to more peripheral parts of the gland.
Age-dependent changes
The pituitary gland volume changes depending on hormonal status and what would be a normal gland in one demographic would be grossly abnormal in another.
Generally speaking, young adults have larger glands than older individuals, and hormonally active individuals (puberty/pregnancy) have the largest glands. These plump glands completely fill the pituitary fossa, and have a convex upper border, whereas older individuals will have a mostly empty pituitary fossa, with a deflated and thinned gland lying on the floor of the sella.
Although one should always be wary of measurements, they can serve to quantify what may otherwise seem overly subjective impressions. These are reasonable maximal figures for the height of the gland:
- children (<12 years): 6 mm (upper surface flat or slightly concave)
- puberty: 10 mm (upper surface convex; more striking in females)
- young adult
- male: 8 mm
- female: 9 mm
- pregnancy: 12 mm
- older adult (>50 years): gradually decreases in size
Systematic approach to interpretation
As with all studies, having a systematic approach to the pituitary region is essential if subtle lesions are to be detected. There is no single correct way to do this, and what is presented is merely a personal approach.
Key structures to identify and assess in every study include:
- pituitary gland including posterior pituitary bright spot and infundibulum
- optic nerves, chiasm, and tracts
- diaphragma sellae and boundaries of the pituitary fossa
- boundaries of the cavernous sinus and Meckel's cave
- internal carotid arteries and branches
- dynamic enhancement of the pituitary
The pituitary gland itself should be examined to ensure that it is age-appropriate in size and normal in signal (see above). The infundibulum should be midline and the posterior pituitary bright spot should be sought, although it is not always visible (ectopic posterior pituitary should be carefully sought in those patients where a normal posterior pituitary bright spot is not evident).
The dynamic enhanced coronal images should be viewed in such a way as to view the wash in of contrast at each location. Depending on the PACS system used and the scanning protocol this can be tricky.
The optic nerves, optic chiasm, and optic tracts should be carefully assessed as even small lesions can lead to visual symptoms, which are a common indication for imaging of this area. The relationship of the chiasm to the pituitary is important and a prefixed (located above the tuberculum sellae) or postfixed (located above the dorsum sellae) chiasm should be identified .
Extreme care should be taken in ensuring that there are no compressive lesions such as a 2-3 mm meningioma. The optic nerves should be followed as far anteriorly as possible on coronal T2 images (if obtained) to assess for the presence of increased signal within the nerve.
Following this, the boundaries of fossa should be examined to ensure that the fossa is not enlarged or eroded (previous mass, hydrocephalus, intracranial hypertension). At this time, the bone marrow signal in the clivus should be assessed (see: normal bone marrow signal of the clivus).
The cavernous sinuses and Meckel's caves should be examined for symmetry and normal anatomy. The visible arteries should all be inspected for obvious aneurysms or malformations; this is best done on T2 weighted imaging if provided. Although no dedicated arterial imaging is present, finding an asymptomatic aneurysm can be a life-saving event. In contrast, missing an obvious aneurysm which later ruptures is a tragedy. Particularly relevant regional aneurysms include anterior communicating artery aneurysms, medially projecting "carotid cave" aneurysm, superiorly projecting ophthalmic artery aneurysms, terminal internal carotid artery aneurysms, posterior communicating artery aneurysms and basilar tip aneurysms.
It is also crucial to identify an aberrant course of the carotid or other aberrant vessels, especially if surgery is likely.
Finally, the rest of the imaged brain should be reviewed for unexpected findings.
Pituitary masses
Assessment of pituitary masses is simplified by taking into consideration the overall pattern (both location, morphology and signal) as well as looking for specific signs.
Patterns
Masses of the pituitary and immediate surrounds present in only a limited number of patterns, which are helpful in narrowing the differential. The two main groups to think of are patterns of morphology and patterns of location.
Patterns of morphology:
- solid and enhancing pituitary region mass
- mixed cystic and solid pituitary region mass
- cystic pituitary region mass
Pattern of location:
- purely intrasellar pituitary mass
- purely suprasellar
- both supra and intrasellar
A couple of additional coexisting patterns which are worth considering are:
- pituitary region mass with intrinsic high T1 signal
- abnormal enhancement/bulkiness of the pituitary infundibulum
Helpful signs
In addition to identifying the dominant imaging pattern, close attention to a number of signs can dramatically aid you in narrowing the differential:
What clinicians want to know
In addition to a general description of any identified mass and the likely diagnosis, there are a number of features which should be specifically commented upon, especially if you believe surgery is likely to be indicated. These include:
- mass
- size in three dimensions
- presence of necrotic/cystic areas
- size of diaphragmatic opening and size of the suprasellar component:
- a narrow waist of the tumor where it passes through the diaphragm may limit the amount of tumor which can be removed via a transsphenoidal approach and whether the tumor will come down at surgery with Valsalva or air into a lumbar drain
- presence of prolapse of the suprasellar membrane (arachnoid):
- this occurs in front of the tumor (visible as a little cleft of CSF in front of the mass)
- presence of this space increases the likelihood of an intraoperative CSF leak
- presence of invasion into the cavernous sinus/clivus/sphenoid sinus/orbit
- location of normal pituitary tissue and infundibulum in relation to the mass
- vessels
- medially located or aberrant carotid arteries
- aneurysms or other visible vascular anomalies especially in the cavernous sinuses
- entering an artery transsphenoidally will not bode well for the patient, the surgeon or the radiologist
- bone
- size of the bony sella, expanded or not, is useful, gives you an idea of the size of the surgical corridor
- degree of pneumatization of the sphenoid, location of the sphenoid septum and any anomalous sinus anatomy
- this is best assessed by CT but is visible also on post-contrast coronal T1 images
- the location of sphenoid septum helps guide the transsphenoidal approach and ensures that the pituitary fossa is entered rather than adjacent cavernous sinus or orbit
- bony dehiscence over the carotid arteries in the sphenoid (better seen on CT)
- presence of florid sinus disease, nasal polyps, septal spurs, etc
Siehe auch:
- Tuberkulose
- Meningeom
- Rathke Zyste
- Hirnmetastase
- Pilozytisches Astrozytom
- Raumforderungen des Clivus
- Aneurysma
- Chordom
- Hypophyse
- Tumoren der Hypophysenregion
- Makroadenom Hypophyse
- Teratom
- intrakranielle Lipome
- Chiasma opticum
- ektope Neurohypophyse
- verdickter Hypophysenstiel
- Kraniopharyngeom
- Nervus opticus
- Germinom
- Sinus cavernosus
- dritter Ventrikel
- Mikroadenom Hypophyse
- Keimzelltumor
- Hypophysenadenom
- Erdheim-Chester-Erkrankung
- Opticusgliom
- hypothalamisches Hamartom
- hypothalamic lesions
- pituitary region mass with intrinsic high T1 signal
- intrakraniale Teratome
- skeletale Manifestationen der Langerhanszell-Histiozytose
- cystic meningioma
- solid and enhancing pituitary region mass
- Epidermoid
- normal bone marrow signal of the clivus
- intrakranielle Dermoidzyste
- Histiozytose
- Cisterna chiasmatica
- Granularzelltumor
- mixed cystic and solid pituitary region mass
- Pituizytom
- purely intrasellar pituitary mass
- zystische Läsionen der Sellaregion
- sakkuläre zerebrale Aneurysmata
- Spindelzell-Onkozytom der Hypophyse
- granular cell tumour of the pituitary
- supraselläres Teratom
- suprasellar lipoma
- Xanthogranulom der Hypophyse
- SATCHMO
- supraselläres Germinom
- cleft cyst
- hypothalamic astrocytoma / glioma
- meningioma, metastasis
- lymphozytäre Hypophysitis
- Metastasen in der Hypophyse

 Assoziationen und Differentialdiagnosen zu Pituitary MRI (an approach):
Assoziationen und Differentialdiagnosen zu Pituitary MRI (an approach):