tumefaktive Demyelinisierung




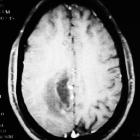





Tumefactive demyelinating lesion (TDL), also sometimes referred to as monofocal acute inflammatory demyelination (MAID), is a locally aggressive form of demyelination, usually manifesting as a solitary lesion (or sometimes a couple of lesions) greater than 2 cm that may mimic a neoplasm on imaging.
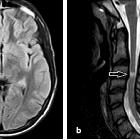
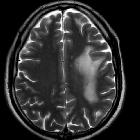
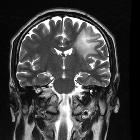
On imaging, they usually present with relatively little mass effect or surrounding edema, contrast enhancement in an open-ring pattern, high ADC values, and low relative cerebral blood volume (rCBV).
Epidemiology
As is the case with multiple sclerosis, and other demyelinating diseases, tumefactive demyelination is most frequently encountered in women, usually young middle age (average onset at 37 years of age) .
Unlike acute disseminated encephalomyelitis (ADEM), tumefactive demyelinating lesions are usually not post-infective. Additionally, although patients with multiple sclerosis can develop large tumefactive demyelinating plaques (which have very similar appearances - see tumefactive multiple sclerosis), patients who present with a solitary tumefactive demyelinating lesion infrequently go on to develop multiple sclerosis (MS) .
Clinical presentation
Patients present with symptoms atypical for multiple sclerosis such as focal neurologic deficits, seizures, and/or aphasia . Most do not progress to multiple sclerosis . In some instances, patients can deteriorate rapidly and succumb to illness (e.g. acute malignant Marburg variant of MS).
Radiographic features
CT
Tumefactive demyelinating lesions appear as a large hypoattenuating lesion with ill-defined ring enhancement, central necrosis, perilesional edema and minimal mass effect .
MRI
The International Magnetic Resonance Imaging in MS Collaboration categorizes the different MRI appearances of tumefactive demyelination:
- ring-enhancing
- diffusely infiltrative
- megacystic
- Balo-like
Tumefactive demyelinating lesions tend to be large but with relatively little mass effect or surrounding edema. Centrally located dilated veins have also been observed within these lesions .
- T1 C+ (Gd)
- about half of tumefactive demyelinating lesions demonstrate contrast enhancement
- the enhancement pattern is usually in the form on an open ring and the incomplete portion of the ring is on the grey matter side of the lesion
- perfusion imaging
- helps differentiate tumefactive demyelinating lesions from the main differential considerations; high-grade gliomas and lymphomas
- mean relative cerebral blood volume within tumefactive demyelinating lesions have been found to be substantially less than in high-grade gliomas and lymphomas
- diffusion imaging (DWI)
- can be less helpful in differentiating tumefactive demyelinating lesions from tumors, as necrotic neoplasms may display a similar increase in apparent diffusion coefficient (ADC)
- however, diffusion imaging can help differentiate ring-enhancing tumefactive demyelinating lesions from cerebral abscesses
- while the former show mildly increased ADC, the latter demonstrate restricted diffusion
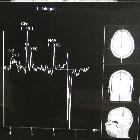
- MR spectroscopy
- beta, gamma glutamate/glutamine (β,γ-Glx) has been shown to be specific to tumefactive demyelinating lesions
- elevation of choline and lactate are supportive of tumefactive MS, but not specific
- the pattern can otherwise be indistinguishable from that of neoplasms (decreased NAA/Cr ratio, increased Cho/Cr ratio, and variable lactate and lipid peaks)
Differential diagnosis
General imaging differential considerations include:
- high-grade glioma (e.g. GBM)
- enhancement is usually a complete ring around central necrosis
- prominent surrounding vasogenic edema
- may have non-enhancing tumor
- CNS lymphoma
- vivid usually solid enhancement, without central non-enhancement (except sometimes in immunocompromised individuals)
- cerebral infective process: cerebritis or cerebral abscess
- restricted diffusion prominent in central liquid component
Practical points
- often there is no evidence of established multiple sclerosis, and many patients do not go onto to develop MS
- tumefactive demyelination is not necessarily benign, and patients can have a fulminant course ending in demise (e.g. Marburg variant of MS)
- lesions are centered on white matter and involve subcortical U-fibers
- less mass effect than expected for size
- incomplete leading edge enhancement is characteristic
- CBV is lower than in tumors
Related video
Siehe auch:
- Hirnabszess
- Neurosarkoidose
- Encephalomyelitis disseminata
- ZNS Lymphom
- Tumefaktive Multiple Sklerose
- inkomplettes Ringenhancement
und weiter:

 Assoziationen und Differentialdiagnosen zu tumefaktive Demyelinisierung:
Assoziationen und Differentialdiagnosen zu tumefaktive Demyelinisierung: